Venlafaxine and Hypertension: What You Need to Know About Blood Pressure Risks
When you take venlafaxine, a serotonin-norepinephrine reuptake inhibitor (SNRI) used to treat depression and anxiety. Also known as Effexor, it works by balancing brain chemicals—but it also affects your body in ways many don’t expect. One of those ways? Raising your blood pressure, the force of blood pushing against artery walls, measured in systolic and diastolic numbers. It’s not a side effect everyone gets, but it’s common enough that your doctor should check it regularly—especially if you’re on higher doses or already have high blood pressure.
Hypertension, chronic high blood pressure that increases risk of heart attack, stroke, and kidney damage. isn’t just a number on a chart. For people taking venlafaxine, it can creep up slowly. Studies show that about 1 in 10 patients on doses above 225 mg per day see a rise in systolic pressure by 10 mmHg or more. That’s not a spike—it’s a steady climb. And if you’re older, have kidney issues, or are already on other meds that affect blood pressure, the risk goes up. The problem? Many people don’t feel anything. No headaches, no dizziness. That’s why monitoring matters more than symptoms.
It’s not just about the drug itself. SNRI medications, a class of antidepressants that increase both serotonin and norepinephrine levels in the brain. like venlafaxine and duloxetine, work by boosting norepinephrine—a chemical that tightens blood vessels. That’s helpful for mood, but it also makes your heart work harder. If you’re taking other stimulants, decongestants, or even some herbal supplements like St. John’s wort, the effect can multiply. Your pharmacist can flag these combos before you even start.
You don’t have to stop venlafaxine if your pressure rises. Often, lowering the dose, switching to a different SNRI, or adding a mild blood pressure med fixes it. But you need to catch it early. That means regular checks—not just when you feel off. If you’ve been on venlafaxine for months and haven’t had your blood pressure checked, ask your doctor. It’s not optional. It’s part of the treatment plan.
Below, you’ll find real-world advice from people who’ve dealt with this exact issue—how to spot early signs, what questions to ask your pharmacist, and how to balance mental health treatment with physical safety. No fluff. No guesses. Just what works.
Severe Hypertensive Crisis from Drug Interactions: What You Need to Know
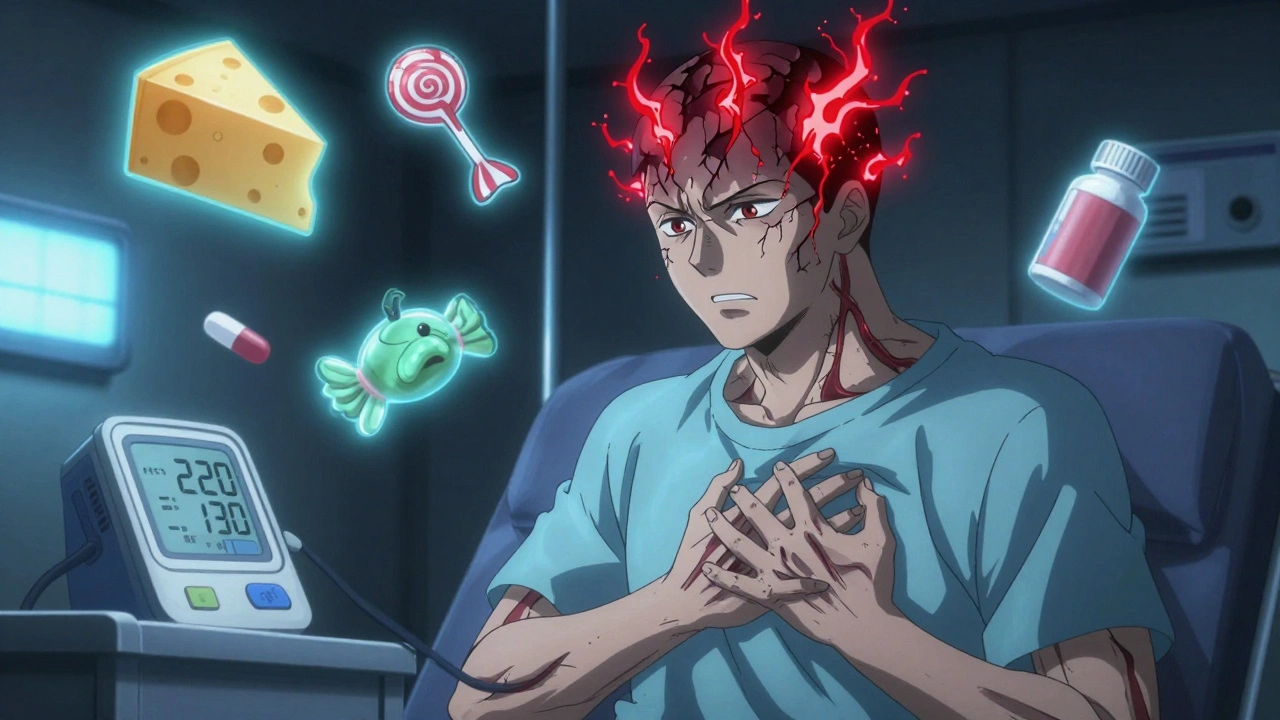
Severe hypertensive crises can be triggered by common drug interactions, including antidepressants, decongestants, and even licorice candy. Learn the hidden risks, warning signs, and how to prevent a life-threatening emergency.
