A severe hypertensive crisis isn’t just a bad headache or a spike on your home monitor. It’s a life-threatening surge in blood pressure-often above 180/120 mmHg-that can tear open blood vessels, trigger a stroke, or shut down your kidneys within minutes. And while many assume high blood pressure is just about stress or salt, a shocking number of these emergencies are caused by something entirely avoidable: drug interactions.
What Exactly Happens During a Hypertensive Crisis?
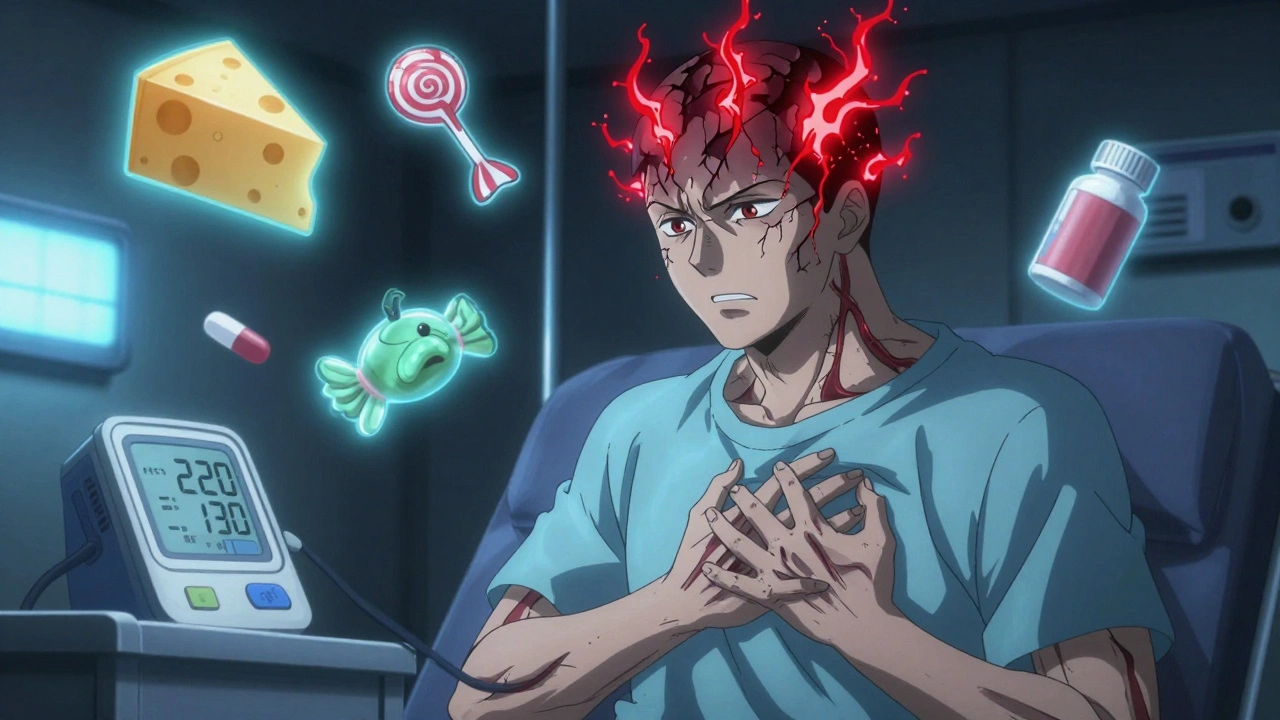
When your blood pressure climbs past 180/120 mmHg, your body’s natural safety systems fail. Blood vessels, already strained, can’t handle the pressure. Tiny leaks form in the lining of arteries. Fluid floods into organs like the brain, heart, and kidneys. This isn’t a slow burn-it’s a sudden rupture in your body’s control system. The difference between a hypertensive urgency and a hypertensive emergency is simple: damage. If your organs are already showing signs of injury-blurred vision, chest pain, confusion, or reduced urine output-you’re in an emergency. And time is critical.
Doctors classify these events into two types. Hypertensive urgency means your pressure is dangerously high but your organs are still intact. You need treatment fast, but you’re not bleeding internally. Hypertensive emergency? That’s when your organs are actively failing. This is what lands people in the ICU. And here’s the scary part: up to 22% of these emergencies are triggered by medications you’re already taking-sometimes even over-the-counter ones.
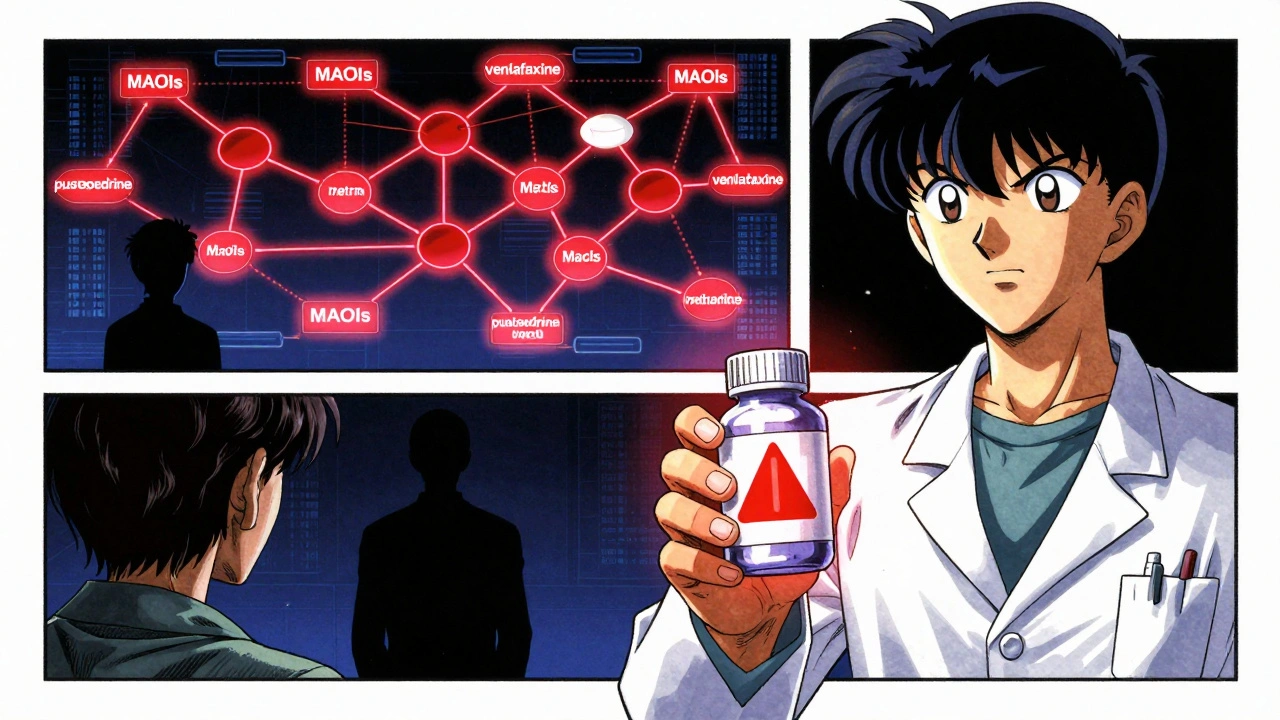
Drugs That Can Trigger a Crisis
Not all medications are created equal when it comes to blood pressure. Some are quietly dangerous when mixed. Take MAOIs-antidepressants like phenelzine or selegiline. They’re effective for treatment-resistant depression, but they come with a deadly warning: avoid aged cheese, cured meats, and red wine. Why? Because these foods contain tyramine. Normally, your body breaks it down. But MAOIs block that process. Tyramine builds up, forces your body to release massive amounts of norepinephrine, and your blood pressure rockets. Case reports show systolic spikes over 250 mmHg in under an hour. One patient described waking up with 220/130 after eating cheddar cheese with their selegiline. Three days in the ICU. Still terrified of cheese.
Then there’s venlafaxine, a common SNRI antidepressant. At doses above 300 mg/day, it can raise diastolic pressure past 90 mmHg. That’s not a minor bump-it’s a red flag. And when combined with stimulants like Adderall or even cold medicines containing pseudoephedrine, the risk jumps 40% compared to historical data. Many patients report headaches or dizziness, but their doctors dismiss it as “anxiety” or “side effects.” By the time they end up in the ER, it’s too late.
Cocaine might seem obvious, but it’s the combo with beta-blockers like propranolol that’s lethal. Cocaine causes vasoconstriction. Propranolol blocks the heart’s ability to compensate. The result? Unopposed alpha-receptor stimulation. Blood vessels clamp shut. Pressure soars. Documented cases show systolic readings above 220 mmHg within 60 minutes.
Even licorice candy is a hidden culprit. Yes, the sweet kind. Licorice contains glycyrrhizin, which mimics aldosterone-a hormone that makes your body hold onto salt and water. This leads to sodium retention, low potassium, and fluid overload. Patients who thought they were just enjoying a snack ended up with blood pressure over 200/110 and potassium levels below 3.0 mmol/L. One woman normalized her pressure in 14 days after quitting licorice candy. No medication. Just stopping the source.
Cyclosporine, used after organ transplants, causes hypertension in up to half of patients. It’s often mistaken for organ rejection, leading doctors to increase the immunosuppressant dose-making the problem worse. In one study, 55% of these cases were misdiagnosed for weeks.
Why This Keeps Happening
You’d think doctors would screen for this. But a 2021 study found only 35% of ER physicians routinely check for drug interactions in patients with severe hypertension. Why? Because the warnings are buried. A 2022 JAMA Internal Medicine analysis found that 78% of high-risk medications have inadequate labels. The FDA now requires black box warnings on MAOIs-but what about the decongestant you bought at the pharmacy? Only 12% of those products carry clear hypertension warnings, according to Consumer Reports.
Patients aren’t to blame entirely. Many don’t know that “natural” doesn’t mean safe. Licorice, St. John’s Wort, ginseng, even some weight-loss supplements can trigger crises. And when patients report symptoms like “I keep getting headaches,” doctors often look for migraines or stress-not drug interactions.
There’s also a gap in monitoring. Patients on cyclosporine or venlafaxine need regular blood pressure checks. But monthly? Biweekly? Few follow that protocol. A Mayo Clinic study showed that using a simple smartphone app called “MAOI Diet Helper” improved dietary adherence by 78%. Technology exists. But it’s not being used.
What You Can Do to Prevent a Crisis
Prevention starts with awareness. If you’re on any of these medications, ask yourself:
- Am I taking an MAOI? If yes, avoid aged cheeses, cured meats, soy sauce, tap beer, and fermented foods.
- Am I on venlafaxine at 225 mg/day or higher? That’s now classified as high risk. Ask your doctor if you need more frequent BP checks.
- Do I use OTC decongestants like pseudoephedrine or phenylephrine? These can spike pressure, especially with antidepressants.
- Do I eat licorice candy or herbal supplements with glycyrrhizin? Stop immediately if you have high blood pressure.
- Am I taking more than five medications? Polypharmacy increases interaction risk by 300% in patients over 65.
Keep a written list of every medication, supplement, and OTC product you take. Bring it to every appointment-even if you think it’s “not important.”
If you’re on an MAOI, wait at least 4-5 weeks after stopping before starting any new antidepressant. Some guidelines say 2 weeks, but irreversible MAOIs like phenelzine need longer. Don’t guess. Ask your pharmacist.
What to Do If You Suspect a Crisis
Don’t wait. If your blood pressure is above 180/120 and you have any of these symptoms-severe headache, blurred vision, chest pain, shortness of breath, nausea, or confusion-go to the ER immediately. Don’t call your doctor. Don’t wait for an appointment. Call 911.
In the hospital, treatment depends on the cause. For MAOI-tyramine reactions, IV phentolamine works in 92% of cases within 20 minutes. For cyclosporine-induced crisis, calcium channel blockers like amlodipine are preferred. For cocaine-induced spikes, benzodiazepines and nitroglycerin are first-line. No one-size-fits-all approach.
And here’s something most people don’t know: you can report these reactions. The FDA’s MedWatch program lets patients report adverse drug events. One patient’s report traced their hypertension to daily licorice candy. That report helped update safety guidelines.

The Future Is Here-But Are We Ready?
There’s good news. In early 2023, the FDA approved the first AI-driven decision-support tool designed to flag drug interactions that cause hypertensive crises. In trials, it cut MAOI-related emergencies by 40%. The NIH is now testing a system that analyzes over 15,000 known interactions with 92% accuracy. Genetic testing for CYP2D6 variants can now identify people at 3.2 times higher risk for severe reactions to certain antidepressants.
But technology won’t fix what humans ignore. The real solution is education-for patients and doctors. A 2024 American College of Cardiology guideline now classifies venlafaxine above 225 mg/day as high risk. That’s progress. But if your doctor doesn’t know about it, it doesn’t matter.
Drug-induced hypertensive crises are not rare. They’re preventable. They’re underdiagnosed. And they’re getting worse as antidepressant prescriptions rise and people stack OTC meds without thinking. You have more power than you realize. Know your meds. Ask questions. Speak up. Your life might depend on it.
Can over-the-counter cold medicine cause a hypertensive crisis?
Yes. Decongestants like pseudoephedrine and phenylephrine can sharply raise blood pressure, especially when taken with antidepressants like MAOIs, SSRIs, or SNRIs. Even one dose can trigger a crisis in someone already on high-risk medications. Always check labels for warnings about high blood pressure, and never take these without talking to your doctor or pharmacist first.
Is licorice candy really dangerous for blood pressure?
Yes. Regular consumption of real licorice candy (not the artificial kind) contains glycyrrhizin, which mimics aldosterone and causes sodium retention, low potassium, and fluid overload. This can lead to systolic pressure over 200 mmHg and dangerous electrolyte imbalances. One case study showed a patient’s blood pressure returned to normal within two weeks of stopping licorice-no medication needed.
How long should I wait between stopping an MAOI and starting a new antidepressant?
For irreversible MAOIs like phenelzine or tranylcypromine, wait at least 4 to 5 weeks. For reversible ones like moclobemide, 2 weeks may be enough. Never guess. Always confirm with your prescribing doctor or pharmacist. Mixing these too soon can cause a life-threatening serotonin syndrome or hypertensive crisis.
Can venlafaxine cause high blood pressure even at normal doses?
Yes. While venlafaxine is generally safe at lower doses (below 150 mg/day), it becomes significantly riskier above 225 mg/day. Studies show diastolic pressure rises above 90 mmHg in many patients at doses over 300 mg/day. Even at standard doses, some individuals are sensitive. If you’re on venlafaxine and notice new headaches, dizziness, or nosebleeds, get your blood pressure checked.
What should I do if I think I’m having a hypertensive crisis?
Call 911 or go to the nearest emergency room immediately. Do not wait. Do not call your doctor’s office. A hypertensive emergency can cause stroke, heart attack, or kidney failure within minutes. Symptoms include severe headache, blurred vision, chest pain, shortness of breath, confusion, or nausea. Time is critical-every minute counts.
Final Thoughts
High blood pressure isn’t always about diet or genetics. Sometimes, it’s the medicine you’re taking-or what you’re mixing it with. The most dangerous interactions aren’t the ones you read about in bold print. They’re the ones hidden in the fine print, the OTC aisle, or the “just a little” habit like daily licorice candy. You don’t need to be an expert to save your life. Just be curious. Ask questions. Keep a list. Speak up. Because in a hypertensive crisis, awareness isn’t just helpful-it’s the difference between life and death.

pallavi khushwani
December 6, 2025 AT 23:06Wow. I never thought my daily licorice habit could be this dangerous. I’ve been eating it since college like it’s candy-turns out I was basically doing a slow-motion sodium bomb on my body. Thanks for laying this out so clearly. I’m tossing the whole bag out today.
Akash Takyar
December 7, 2025 AT 22:11While I appreciate the clinical detail presented herein, I must emphasize the necessity of structured patient education protocols. The absence of standardized pharmacovigilance training in primary care settings remains a systemic failure. A multi-disciplinary approach, incorporating pharmacy-led counseling and digital alerts, is imperative to mitigate preventable morbidity.
brenda olvera
December 9, 2025 AT 09:39My abuela used to say ‘everything in moderation’ but she never told me licorice was poison. I’ve been eating it since I was a kid in Mexico City. Guess I’m switching to dark chocolate now. Thanks for the wake-up call 💪
Brooke Evers
December 11, 2025 AT 02:08I’ve been on venlafaxine for five years now, and I’ve had this weird, constant headache for months. My doctor kept saying it was stress or eye strain. I finally got my BP checked last week-it was 178/94. I didn’t even connect it. I’m so glad I read this. I’m calling my pharmacist tomorrow to ask about the dose and what else I might be mixing with it. I’m scared but also relieved I didn’t wait until I collapsed. I think a lot of us just assume our doctors know all this stuff, but honestly? They’re overwhelmed. We have to be our own advocates.
Saketh Sai Rachapudi
December 12, 2025 AT 23:25USA doctors are so lazy they let people die from candy. In India we dont have this problem because we dont take all these pills. If you want to be healthy, eat roti and chilli, not some fancy antidepressant. Stop taking meds and stop being weak. Your body is not broken. You just need discipline.
joanne humphreys
December 14, 2025 AT 08:47This is such an important post. I work in a clinic and see patients every day who don’t realize their ‘natural’ supplements are interacting with their prescriptions. I’ve had people take St. John’s Wort with SSRIs and then panic when they get dizzy. I wish more people knew how common this is. I’ve started handing out little printed cards with common risky combos. It’s simple, but it helps.
Kay Jolie
December 15, 2025 AT 16:01Let’s be real-the pharmaceutical-industrial complex is not designed to inform you, it’s designed to monetize your ignorance. MAOIs? Black box warnings. Licorice? No warning. Why? Because licorice doesn’t have a patent. The real tragedy isn’t the drug interaction-it’s the fact that we’ve outsourced our health literacy to corporations that profit from your confusion. This isn’t about ‘being careful.’ It’s about systemic deception wrapped in a white coat.
Dan Cole
December 15, 2025 AT 16:43Actually, the FDA’s AI tool is not ‘the first’-it’s a rebranded version of a 2018 algorithm developed by Stanford that was shelved due to lack of funding. Also, CYP2D6 testing has been available since 2007, but most insurers won’t cover it unless you’re on three or more psychotropics. And let’s not pretend that ‘asking your pharmacist’ is a viable solution when 70% of pharmacists are overworked and underpaid. This post reads like a TED Talk with footnotes. The problem isn’t awareness-it’s infrastructure. And infrastructure doesn’t care about your blog post.
Billy Schimmel
December 17, 2025 AT 01:26So let me get this straight… I can’t have licorice, cheese, or cold medicine… but I can take 17 pills a day and call it ‘healthy’? Cool. Thanks for the guilt trip.