Transient Ischemic Attack (TIA) – What You Need to Know
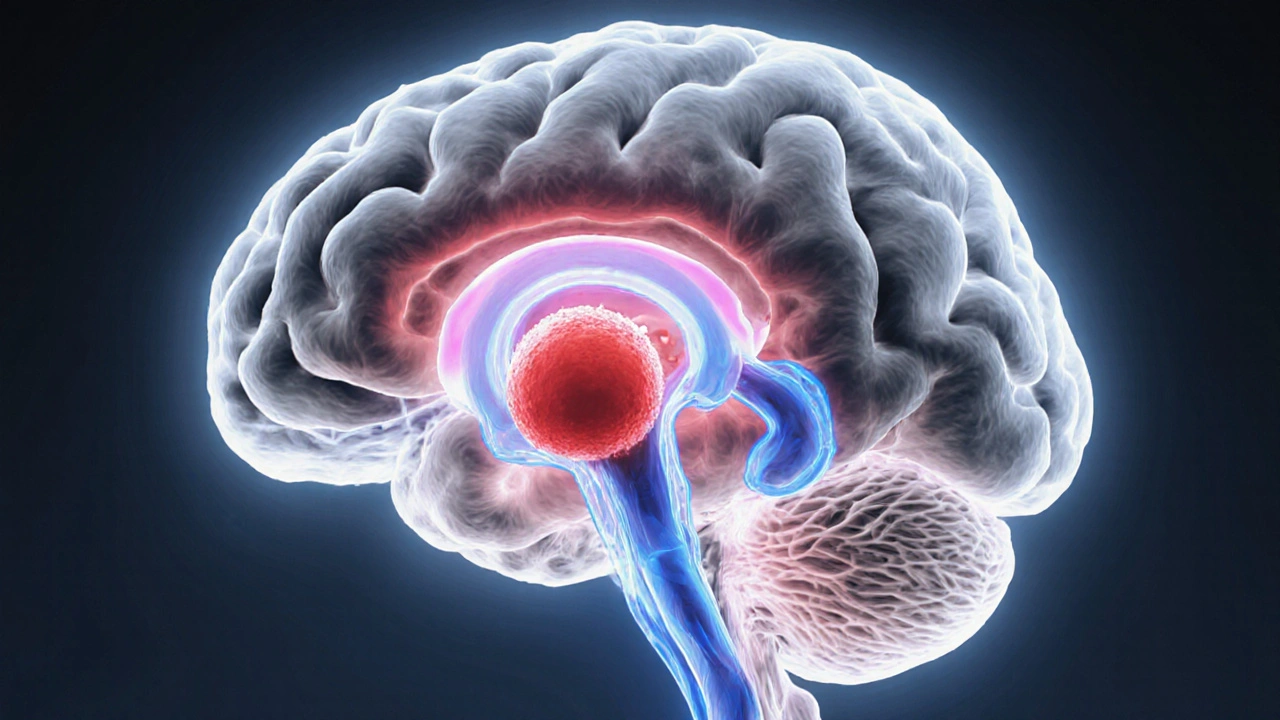
Understanding Transient Ischemic Attack can feel like deciphering a warning alarm for your brain. When you first hear the term, think of a brief, “mini‑stroke” that clears up within minutes. Transient Ischemic Attack, a temporary disruption of blood flow to part of the brain that resolves quickly but signals a serious underlying problem. Also known as a “TIA,” it serves as a red flag that a full‑blown stroke may be on the horizon.
Key Aspects of TIA
One major stroke, a lasting blockage or bleed in the brain that causes permanent damage often follows an untreated TIA. That’s why doctors say a TIA encompasses short‑lived neurological deficits but requires immediate evaluation. The most common symptoms—sudden weakness, slurred speech, or vision loss—last less than 24 hours, usually just a few minutes. If you notice any of these signs, call emergency services right away; early treatment can stop the chain reaction that leads to a stroke.
What pushes a TIA over the edge? risk factors, conditions like high blood pressure, diabetes, high cholesterol, smoking, and atrial fibrillation that increase the chance of blood clots are the main culprits. Think of them as the oil that makes the gears of a clotting system stick together. Managing these factors—through diet, exercise, and medication—cuts the odds of both TIA and subsequent stroke dramatically. Even something as simple as cutting back on salty snacks can lower blood pressure and, in turn, reduce the clot‑forming potential.
When a doctor confirms a TIA, the conversation often turns to anticoagulants, blood‑thinning drugs that prevent clot formation and are commonly prescribed for atrial fibrillation and other heart rhythm disorders. These meds act like a traffic controller, keeping platelets from building up into dangerous clumps. For many patients, especially those with an irregular heartbeat, anticoagulants are the frontline defense that can turn a ticking‑time‑bomb scenario into a manageable condition. However, they need careful dosing and regular monitoring to balance clot prevention with bleeding risk.
Beyond medication, doctors may order imaging tests—like a carotid ultrasound or MRI—to spot narrowing arteries or hidden plaques. This diagnostic step enables them to decide whether a surgical option, such as carotid endarterectomy, is necessary. It’s a clear example of how a TIA influences treatment pathways: the brief event triggers a cascade of tests, lifestyle tweaks, and possibly procedures, all aimed at keeping the brain safe.
In everyday life, recognizing a TIA isn’t just about spotting symptoms; it’s also about understanding your personal risk profile. If you’ve got high blood pressure or a family history of heart disease, keep a symptom diary and share it with your clinician. Simple habits—regular BP checks, quitting smoking, and staying active—add up to a powerful prevention toolkit. Think of each habit as a brick that builds a wall against future strokes.
Below you’ll find a curated set of articles that dive deeper into medication side effects, drug comparisons, and specific health conditions that often intersect with TIA management. From how tamsulosin works to the latest on anticoagulant therapy, these posts give you practical, up‑to‑date information you can apply right away. Let’s explore how each piece fits into the bigger picture of protecting your brain health.
Understanding Different Types of Transient Ischemic Attacks
Learn the main types of Transient Ischemic Attacks, their causes, symptoms, diagnosis, risk factors, and prevention strategies to avoid a future stroke.
