TIA Risk Estimator
Assess Your Stroke Risk
Based on key risk factors discussed in the article, this tool estimates your 90-day stroke risk after a TIA. Results are for informational purposes only.
Your Estimated 90-Day Stroke Risk
Quick Takeaways
- TIAs are brief episodes of brain ischemia that signal a high risk of future stroke.
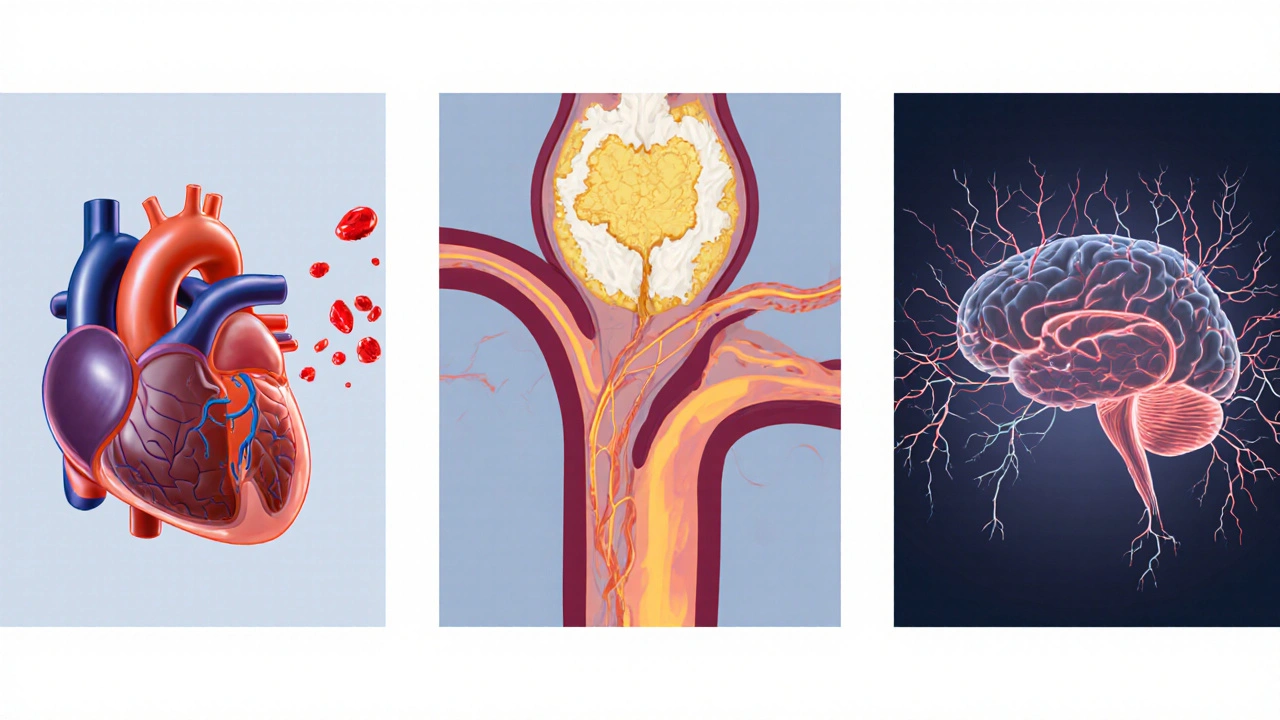
- Three main mechanisms drive TIAs: embolic, atherosclerotic, and small‑vessel (lacunar) disease.
- Symptoms resolve within an hour, but imaging is essential to confirm a TIA and rule out stroke.
- Control of hypertension, diabetes, and cholesterol cuts the recurrence risk dramatically.
- Antiplatelet therapy, lifestyle changes, and timely vascular evaluation are the cornerstones of prevention.
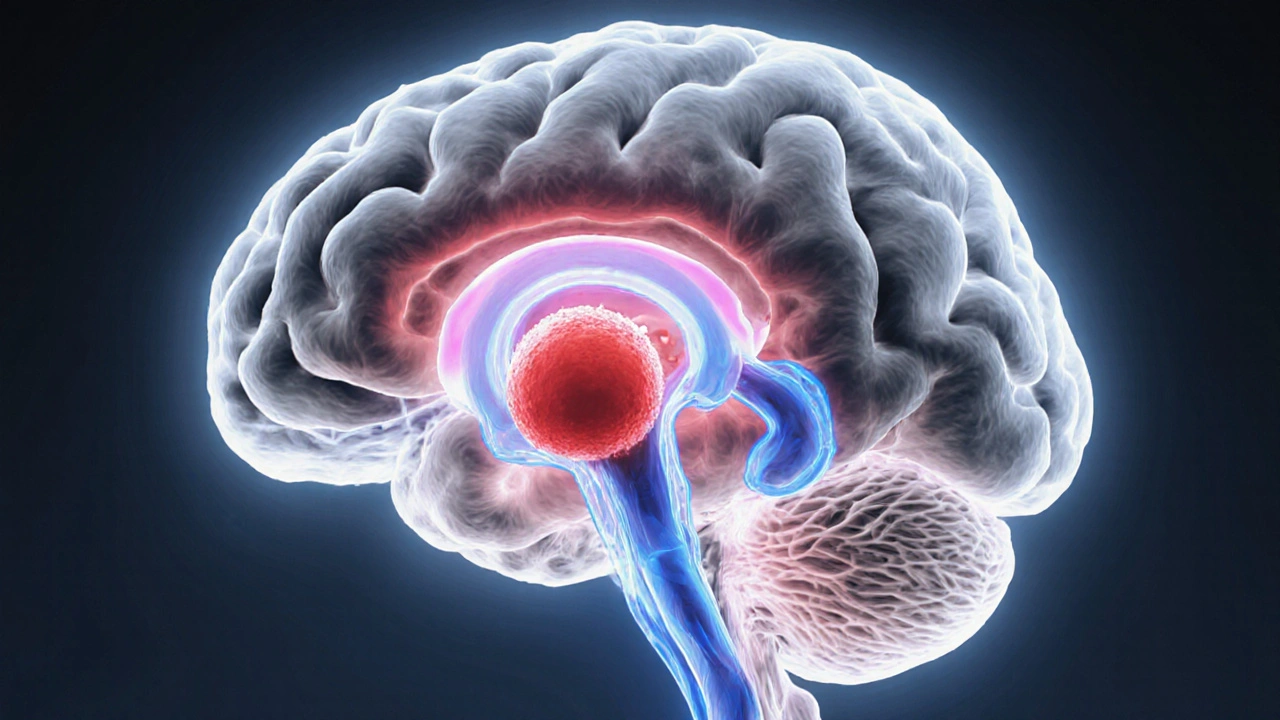
When doctors talk about a Transient Ischemic Attack is a brief neurological episode caused by a temporary reduction in blood flow to part of the brain, they’re describing what’s often called a “mini‑stroke.” Even though symptoms fade quickly, a TIA is a warning bell that a full‑blown stroke is lurking nearby.
What Exactly Is a TIA?
A TIA occurs when a clot or plaque blocks a cerebral artery long enough to cause neurological deficits-such as weakness, speech trouble, or vision loss-but not long enough to cause permanent brain damage. By definition, symptoms last less than 24 hours, and in most modern series they resolve within minutes.
Key attributes of a TIA include:
- Duration: usually under 60 minutes.
- Reversibility: neurological function returns to baseline.
- Risk Indicator: about 10‑20% of patients suffer a stroke within 90 days if the underlying cause isn’t addressed.
Major Types of Transient Ischemic Attacks
Clinicians sort TIAs into three broad mechanisms. Understanding the type helps decide which test and treatment will be most effective.
| Mechanism | Typical Source | Common Symptoms | Preferred Diagnostic Test | First‑Line Prevention |
|---|---|---|---|---|
| Embolic | Cardioembolism (e.g., atrial fibrillation) or proximal artery plaque | Sudden onset, often affecting speech or vision | Transcranial Doppler or MRI with diffusion‑weighted imaging | Anticoagulation for AF, antiplatelet for atherosclerotic sources |
| Atherosclerotic | Carotid artery stenosis or intracranial atherosclerosis | Gradual weakness on one side, facial droop | Carotid duplex ultrasound, CTA/MRA | Statins, antiplatelet agents, possible carotid endarterectomy |
| Small‑vessel (Lacunar) | Hypertensive arteriolosclerosis affecting deep penetrating arteries | Pure motor or sensory deficits, often confined to one limb | MRI with high‑resolution sequences | Strict blood‑pressure control, lifestyle modification |
Symptoms & How They Differ From Stroke
Because TIAs resolve quickly, patients often miss the warning. Typical signs include:
- Sudden weakness or numbness on one side of the body.
- Slurred speech or difficulty understanding language.
- Loss of vision in one eye (amaurosis fugax).
- Dizziness, imbalance, or loss of coordination.
Unlike stroke, the deficit disappears fully. However, the same brain region may be involved, so the pattern of symptoms can give clues about the underlying vessel.
Diagnostic Work‑up
Even after symptoms fade, doctors need objective proof. The core tests are:
- Magnetic Resonance Imaging (MRI) with diffusion‑weighted sequences - catches tiny infarcts that may have occurred.
- CT angiography or MR angiography - visualizes arterial narrowing or occlusion.
- Carotid duplex ultrasound - evaluates Carotid Artery Stenosis is a narrowing of the carotid artery caused by plaque buildup.
- Cardiac monitoring (24‑hour Holter, event recorder) - looks for Cardioembolism is a clot that forms in the heart and travels to the brain, especially atrial fibrillation.
These studies guide whether the patient needs antiplatelet medication, anticoagulation, or a surgical procedure.
Key Risk Factors
Some factors raise the odds of a TIA more than others. The strongest predictor is uncontrolled hypertension is high blood pressure that damages blood‑vessel walls. Others include:
- Diabetes mellitus - high glucose accelerates atherosclerosis.
- Hyperlipidemia - excess LDL cholesterol feeds plaque formation.
- Smoking - promotes endothelial injury.
- Obesity and sedentary lifestyle - worsen all of the above.
- Family history of cerebrovascular disease.
Addressing these modifiable risks cuts the 90‑day stroke risk from roughly 15% to under 5%.

Management and Prevention Strategies
Once the TIA type is known, treatment can be tailored.
- Antiplatelet therapy - aspirin or clopidogrel for atherosclerotic and lacunar TIAs.
- Anticoagulation - warfarin, dabigatran, apixaban, or rivaroxaban for cardioembolic sources such as atrial fibrillation.
- Statin therapy - high‑intensity statins lower LDL and stabilise plaque.
- Blood‑pressure control - aim for <130/80mmHg for most patients; lower targets may be set for diabetics.
- Carotid revascularisation - endarterectomy or stenting when stenosis exceeds 70% and the patient is symptomatic.
- Lifestyle upgrades - quit smoking, adopt a DASH or Mediterranean diet, and exercise at least 150minutes per week.
Follow‑up within 24‑48hours is recommended to confirm that the work‑up is complete and the prevention plan is in place.
When to Call Emergency Services
If any neurological symptom appears and lasts more than a few minutes, treat it as a possible stroke. Call 911 immediately. Time is brain, and early thrombolysis can save tissue.
Common Misconceptions
- “If it went away, it’s nothing.” - false. The symptom’s disappearance doesn’t erase the underlying vessel problem.
- “TIA only happens to older adults.” - while risk rises with age, younger patients with clotting disorders or congenital heart disease can also experience TIAs.
- “Taking aspirin after a TIA is enough.” - aspirin is a good start, but many patients need anticoagulation or surgical intervention based on cause.
Frequently Asked Questions
How long does a TIA usually last?
Most TIAs resolve within 5‑10 minutes, and virtually all end before 60 minutes. Historically the cutoff was 24 hours, but modern imaging shows that symptoms lasting longer than an hour usually indicate a small stroke.
Can a TIA happen more than once?
Yes. Recurrent TIAs are common, especially if risk factors aren’t controlled. Each new event raises the odds of a subsequent stroke.
Is imaging always required after a TIA?
Guidelines recommend MRI with diffusion‑weighted imaging within 24‑48hours to rule out a silent infarct and to guide therapy. If MRI isn’t available, a CT scan plus vascular imaging is acceptable.
What lifestyle changes reduce TIA risk the most?
Quitting smoking, maintaining a healthy weight, eating a diet rich in fruits, vegetables, and omega‑3 fatty acids, exercising regularly, and keeping blood pressure and cholesterol in target ranges have the biggest impact.
When is carotid surgery recommended?
If the carotid artery is narrowed by 70% or more on the side that caused the TIA, and the patient is a good surgical candidate, endarterectomy or stenting significantly lowers future stroke risk.
Understanding the different types of Transient Ischemic Attack empowers patients and clinicians to act fast, run the right tests, and start the best preventive therapy before a full‑blown stroke strikes.

Lydia Conier
October 12, 2025 AT 06:24Understanding the different TIA presentations can really help patients spot warning signs early.
It’s important to know that symptoms may resolve within minutes, but the underlying risk stays.
Keeping track of personal risk factors makes the calculator even more useful.
ruth purizaca
October 13, 2025 AT 12:57One would think a simple risk estimator could be more nuanced, yet it reduces a complex vascular picture to check‑boxes.
Such reductive tools risk giving a false sense of security for those who need thorough evaluation.
Shelley Beneteau
October 14, 2025 AT 16:44When it comes to transient ischemic attacks, the variability in symptom duration is fascinating.
Some patients experience fleeting vision loss, while others report brief speech difficulties.
The underlying mechanisms often involve small emboli that dissolve quickly.
Identifying these patterns can guide clinicians toward appropriate imaging.
It also underscores why lifestyle modification remains a cornerstone of prevention.
Sonya Postnikova
October 15, 2025 AT 20:31Love how the tool nudges you to talk to your doc after you get a number! 😊
Even a rough estimate is better than flying blind.
Stay proactive and keep those risk factors in check.
Anna Zawierucha
October 17, 2025 AT 00:17Ah yes, because a flashy calculator magically fixes hypertension and smoking habits.
Colorful graphics won’t replace real lifestyle changes, but they do make the data look pretty.
Lolita Rosa
October 18, 2025 AT 04:04Honestly, this looks like a cheap app.
Matthew Platts
October 19, 2025 AT 07:51Even a basic tool can spark a conversation with a doctor about stopping smoking.
Matthew Bates
October 20, 2025 AT 11:37The presented risk estimator is a simplistic linear model that aggregates age, hypertension, diabetes, smoking status, and carotid stenosis into an additive score.
Such an approach neglects the well‑documented interaction effects between these variables, for instance, the synergistic risk elevation when hypertension co‑exists with diabetes.
Furthermore, the binary categorisation of risk factors fails to capture the continuum of disease severity, such as the degree of carotid narrowing or the quantitative burden of glycated hemoglobin.
Current guidelines from the American Heart Association recommend incorporating multivariate logistic regression models that adjust for confounders and employ calibrated probability estimates.
Relying solely on a point‑based system may under‑estimate risk in younger patients with multiple mild risk factors and over‑estimate it in elderly individuals with isolated hypertension.
In addition, the tool does not account for recent atrial fibrillation episodes, which are a prominent source of embolic TIAs.
It also omits the consideration of prior TIA frequency, medication adherence, and lipid profile, all of which materially influence short‑term stroke probability.
The absence of a confidence interval around the displayed percentage further limits clinical interpretability, as point estimates can be misleading without an appreciation of statistical uncertainty.
While the interface is user‑friendly, clinicians must be cautious not to substitute this calculator for comprehensive vascular assessment, including neuroimaging, cardiac monitoring, and laboratory workup.
Patients should be counselled that the output is an illustrative figure, not a definitive prognostic metric.
In practice, integrating this calculator into a broader decision‑support framework, perhaps linked to electronic health records, could enhance its utility.
Nonetheless, the current iteration serves as an educational adjunct rather than a definitive risk stratification tool.
Future iterations should incorporate machine‑learning algorithms that dynamically weight risk factors based on large population datasets.
Such refinement would improve calibration and discrimination, aligning the estimator with contemporary evidence‑based practice.
Kasey Mynatt
October 21, 2025 AT 15:24Thanks for highlighting the limitations; it’s crucial that users don’t treat the number as gospel.
Encouraging patients to discuss the results with their physician can lead to a more tailored prevention plan.
Keep the tone supportive and the facts clear – that’s how we empower people.
Shriniwas Kumar
October 22, 2025 AT 19:11From a global health perspective, the inclusion of carotid stenosis as a binary variable is a rudimentary proxy for atherosclerotic burden.
In many low‑resource settings, duplex ultrasonography may be unavailable, necessitating reliance on clinical risk scoring.
Thus, a culturally adapted algorithm that accounts for regional epidemiology, such as higher prevalence of intracranial atherosclerosis, would enhance applicability.
Moreover, the tool could benefit from integrating South‑Asian specific metabolic risk factors, like heightened insulin resistance at lower BMI thresholds.