Torsades de Pointes: Causes, Risks, and Medications That Trigger It
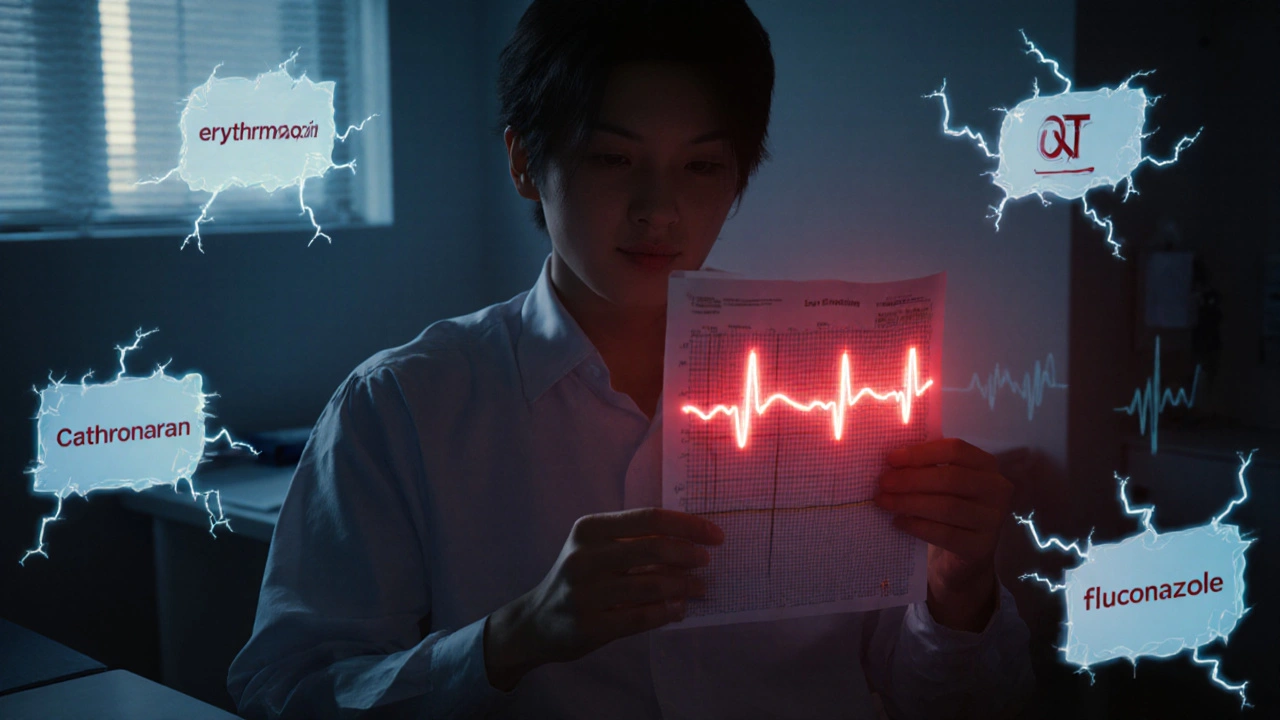
When your heart’s electrical system goes haywire, it can trigger torsades de pointes, a specific type of life-threatening irregular heartbeat that appears as a twisting pattern on an ECG. Also known as polymorphic ventricular tachycardia, it doesn’t just flutter—it can collapse into cardiac arrest if not caught fast. This isn’t some rare glitch you hear about in medical dramas. It happens in real people, often because of a medication they took without knowing the risk.
What makes torsades de pointes so dangerous is how often it’s tied to something preventable: QT prolongation, a delay in the heart’s electrical recovery phase that shows up as a longer line on an ECG. Many common drugs—antibiotics, antidepressants, anti-nausea meds, and even some heart pills—can stretch that line out. A single dose of an off-label antibiotic or a new prescription for migraines might be all it takes. People with low potassium, low magnesium, or existing heart disease are at higher risk, but even healthy folks aren’t immune.
It’s not just about one drug. The real danger comes from combinations. Take a QT-prolonging antibiotic with a diuretic that drains your electrolytes? That’s a recipe for trouble. Or mix an antipsychotic with an antiarrhythmic meant to fix another rhythm problem? You might accidentally trigger the very thing you’re trying to treat. That’s why doctors check your meds, your labs, and your ECG before prescribing certain drugs. And why you should always ask: Could this mess with my heart rhythm?
Some of the most common culprits include macrolide antibiotics like azithromycin, antifungals like fluconazole, certain antidepressants like citalopram, and antiarrhythmics like sotalol and dofetilide. Even older drugs like chloroquine or haloperidol still show up in cases. It’s not that these drugs are bad—they work well for their intended use. But they carry a quiet risk that doesn’t show up in symptoms until it’s too late.
What you’ll find in the posts below isn’t just a list of drugs. It’s a practical look at how medications like losartan-hydrochlorothiazide, Mestinon, or even common sleep aids can interact with your heart’s electrical system. Some posts dig into how DOACs behave in obese patients, others compare antibiotics or anti-inflammatories that might quietly affect your QT interval. You won’t find fluff. Just clear, real-world connections between the pills you take and the rhythm your heart keeps.
Methadone and QT-Prolonging Drugs: What You Need to Know About Arrhythmia Risk
Methadone can prolong the QT interval and increase the risk of dangerous heart rhythms, especially when combined with other QT-prolonging drugs. Learn who’s at risk, which medications to avoid, and how to stay safe.
