TIA Treatment: What You Need to Know
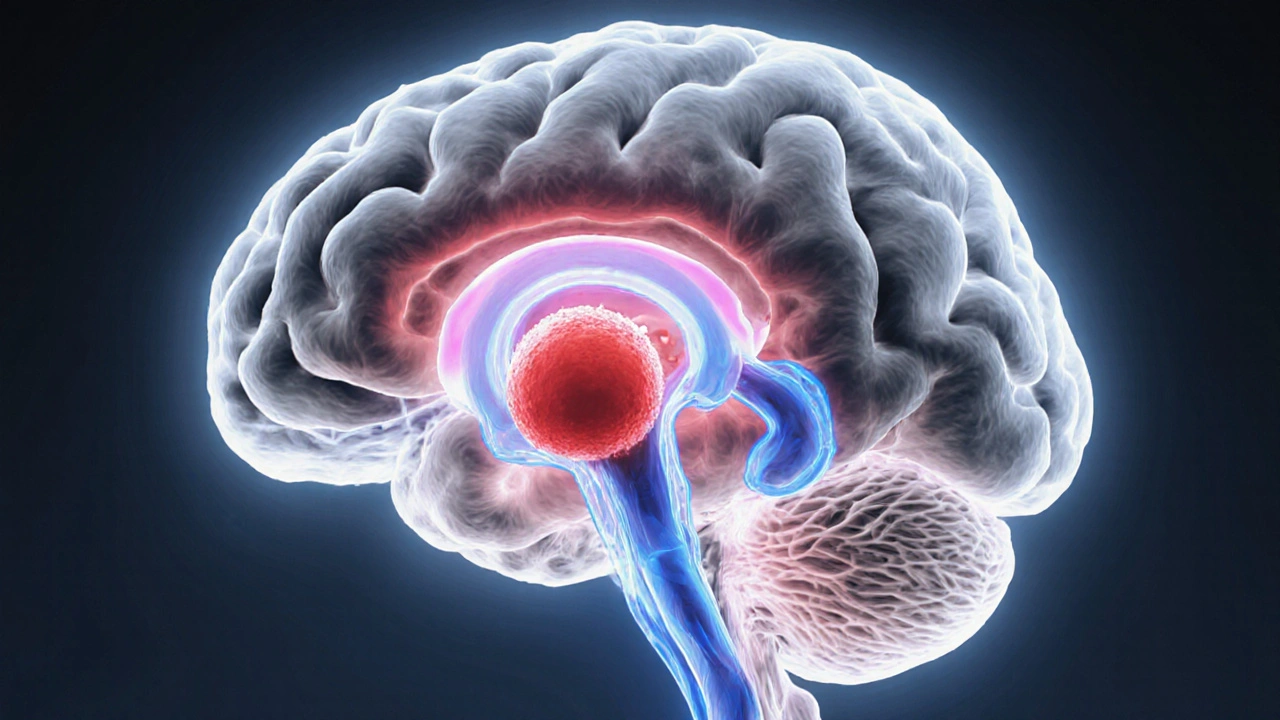
When dealing with TIA treatment, the medical approach used to prevent a full‑blown stroke after a transient ischemic attack. Also known as mini‑stroke therapy, it focuses on quickly restoring blood flow, reducing clot risk, and addressing underlying vessel problems. Understanding this helps you act fast and cut long‑term damage.
TIA treatment isn’t one‑size‑fits‑all. It blends medication, lifestyle tweaks, and sometimes surgery. The first pillar is antiplatelet therapy, drugs that stop platelets from sticking together and forming clots. Common choices include aspirin and clopidogrel. By keeping platelets from aggregating, antiplatelet therapy directly lowers the chance that a tiny blockage turns into a permanent stroke. This link—TIA treatment includes antiplatelet therapy—forms a core part of the prevention strategy.
When platelets aren’t the only culprits, clinicians turn to anticoagulants, blood‑thinning medications that interfere with clot‑forming proteins. Warfarin, dabigatran, and the newer DOACs belong here. Anticoagulants are especially useful if the TIA stems from atrial fibrillation or a cardio‑embolic source. The semantic triple—anticoagulants reduce stroke risk after a TIA—captures why doctors may prescribe them alongside or instead of antiplatelet drugs, depending on the patient’s heart rhythm and clotting profile.
Vessel health matters just as much as medication. carotid artery disease, narrowing or plaque buildup in the main neck arteries that supply the brain, often triggers TIAs. When imaging shows a 70 %+ blockage, surgeons may recommend carotid endarterectomy or stenting. This procedure removes plaque, restores normal flow, and directly tackles the source of many TIAs. The relationship—carotid artery disease influences TIA treatment decisions—explains why imaging tests like ultrasound or CTA are routine after a mini‑stroke.
Key Components of Effective TIA Management
Beyond drugs and surgery, risk‑factor control is a must‑have. High blood pressure, diabetes, and high cholesterol each raise the odds of another TIA or a full stroke. Lifestyle changes—regular aerobic exercise, a Mediterranean‑style diet, and quitting smoking—act as non‑pharmacologic extensions of TIA treatment. Think of them as the “maintenance crew” that keeps the vascular system running smoothly after the acute phase.
Another essential piece is patient education. People who recognize TIA symptoms (sudden weakness, speech trouble, vision loss lasting less than 24 hours) can seek care within the critical “golden hour.” Early evaluation allows doctors to start antiplatelet or anticoagulant therapy quickly, often before the brain suffers lasting injury. This speed‑to‑treatment pathway directly connects symptom awareness to better outcomes, reinforcing the overall goal of TIA treatment.
Finally, follow‑up monitoring ties everything together. Regular check‑ups, repeat imaging, and blood‑test panels ensure that the chosen therapy remains effective and safe. Adjusting dosages, swapping meds, or scheduling a procedure depends on how the patient’s risk profile evolves over weeks and months. This continuous loop—TIA treatment requires ongoing assessment—helps keep the prevention plan on track.
All of these elements—medication, vascular intervention, lifestyle overhaul, and vigilant follow‑up—make up a comprehensive approach. Below you’ll find a curated list of articles that dig deeper into each area, from detailed drug comparisons to step‑by‑step guides on buying affordable generics. Dive in to sharpen your understanding and take confident steps toward protecting your brain health.
Understanding Different Types of Transient Ischemic Attacks
Learn the main types of Transient Ischemic Attacks, their causes, symptoms, diagnosis, risk factors, and prevention strategies to avoid a future stroke.
