Senior Drug Adjustments: What You Need to Know About Medication Changes for Older Adults
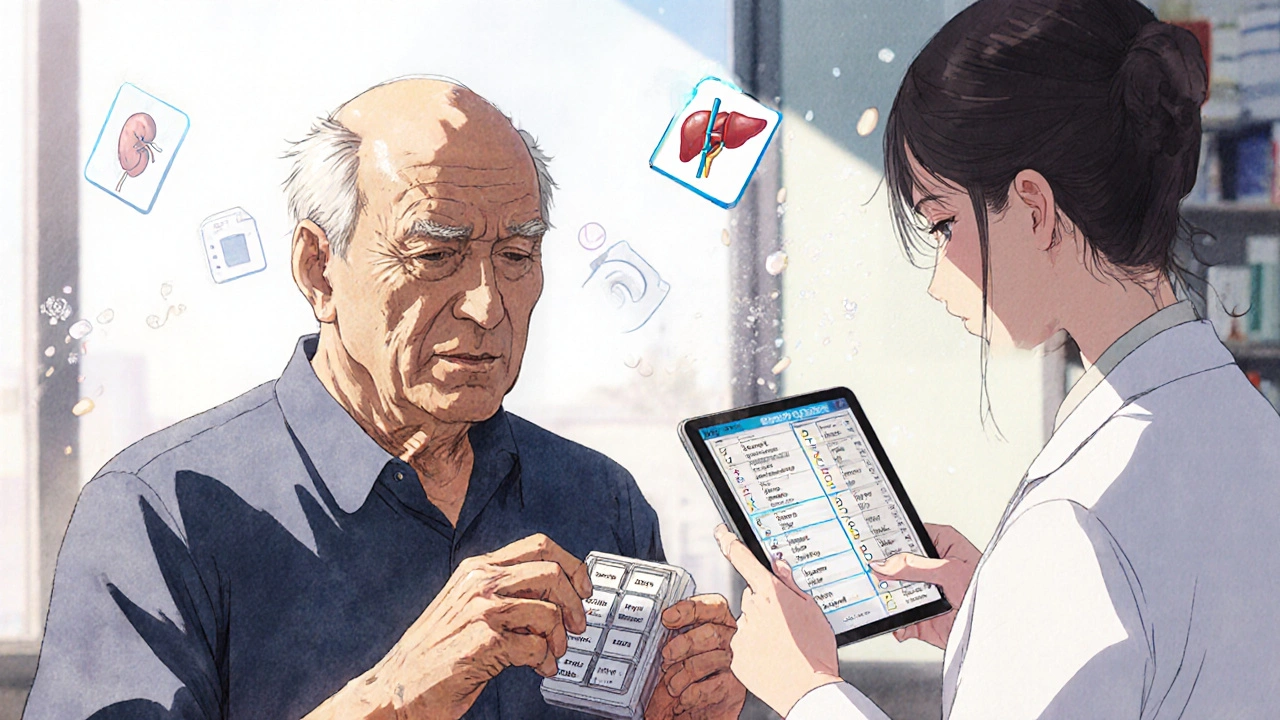
When you’re over 65, your body doesn’t process drugs the same way it did at 30. Senior drug adjustments, changes in medication type, dose, or frequency made to account for aging physiology. Also known as geriatric dosing, these adjustments aren’t optional—they’re lifesaving. As people age, their kidneys and liver slow down, body fat increases, and muscle mass drops. That means drugs stick around longer, build up in the system, and can turn harmless doses into dangerous ones. A pill that was fine at 50 might cause confusion, falls, or heart trouble at 75.
One of the biggest risks? Polypharmacy, taking five or more medications at once. Also known as medication overload, it’s common in seniors managing diabetes, high blood pressure, arthritis, and sleep issues—but each added drug raises the chance of a bad interaction. Take meclizine, a common vertigo drug. Also known as an antihistamine for dizziness, it’s often prescribed to older adults, but it causes drowsiness and dry mouth, which can lead to falls or urinary retention. Combine it with a blood pressure pill like losartan-hydrochlorothiazide, a combination used to lower blood pressure. Also known as an ARB-diuretic combo, and you’ve got a recipe for low blood pressure, dizziness, and kidney strain. These aren’t hypotheticals. Real people end up in the ER because their meds weren’t rechecked after 70.
It’s not just about what you’re taking—it’s about how your body changes. Your liver breaks down drugs slower. Your kidneys flush them out less efficiently. Even something as simple as acetaminophen, the active ingredient in Tylenol. Also known as paracetamol, it’s safe for most, but in seniors, the liver’s ability to process it drops, increasing overdose risk—even at regular doses. That’s why doctors need to lower doses, switch to safer alternatives, or drop drugs entirely. The FDA requires generics to match brand names in strength, but it doesn’t change how aging affects absorption. A 500mg tablet of Tylenol might be fine for a 40-year-old but risky for a 78-year-old with mild kidney disease.
And it’s not just pills. Supplements like kava, a natural anxiety remedy. Also known as Piper methysticum, can cause liver damage—especially when mixed with statins, antidepressants, or even common painkillers. Many seniors take kava thinking it’s safe because it’s "natural." But nature doesn’t care about your age or your other meds. The same goes for melatonin, a sleep aid often used by older adults. Also known as a hormone supplement, it can interfere with blood pressure control and interact with anticoagulants like DOACs.
There’s no one-size-fits-all fix. But the right senior drug adjustments can mean the difference between staying independent and ending up in the hospital. That’s why the posts below cover real cases: how DOAC dosing, anticoagulants like apixaban and rivaroxaban. Also known as new oral blood thinners, need to be lowered in frail seniors, why tamsulosin, a BPH drug. Also known as an alpha-blocker, can cause dangerous drops in blood pressure, and how methadone, used for pain and addiction. Also known as a QT-prolonging opioid, can trigger heart rhythm problems when combined with other meds. These aren’t theory—they’re daily realities for older patients and their doctors.
Below, you’ll find practical guides on how to spot risky combinations, when to ask for a med review, and which alternatives actually work for seniors. No fluff. No marketing. Just what you need to keep your meds safe as you age.
Medication Dosage Adjustments for Aging Bodies and Organs
Aging changes how your body handles medicine. Learn why seniors need lower doses, which drugs are most dangerous, and how to avoid harmful side effects through proper medication adjustments.
