High Blood Pressure Emergency: Signs, Risks, and What to Do Now
When your blood pressure spikes to dangerous levels, it’s not just a number—it’s a high blood pressure emergency, a life-threatening condition where blood pressure rises so high it damages organs. Also known as a hypertensive crisis, this isn’t something you can wait out. It requires immediate action to prevent stroke, heart attack, or kidney failure. Unlike routine high blood pressure, which builds over years, a high blood pressure emergency happens fast—often without clear warning, but sometimes with unmistakable symptoms.
There are two types: hypertensive urgency, when blood pressure is extremely high but organs aren’t yet damaged, and hypertensive emergency, when high pressure is already harming the brain, heart, kidneys, or eyes. The difference? Time. In urgency, you have hours to lower pressure safely. In emergency, you need minutes. Symptoms like severe headache, blurred vision, chest pain, shortness of breath, or confusion aren’t just discomfort—they’re red flags. Many people ignore them because they feel fine otherwise, but that’s exactly when the damage is already starting.
What triggers this? Skipping meds, sudden stress, drug interactions, or even a bad reaction to cold medicine. People with untreated or poorly controlled high blood pressure are at highest risk, but even those who think they’re managing it can slip through the cracks. Studies show nearly 1 in 5 hypertensive emergencies happen because someone stopped their meds without talking to a doctor. Others develop it after using decongestants, stimulants, or even some herbal supplements that silently raise pressure.
Knowing what to do saves lives. If your reading is over 180/120 and you have symptoms, don’t wait for your next appointment. Call 911. Don’t try to lower it yourself with home remedies or extra pills—that can crash your pressure too fast and cause more harm. Emergency rooms have protocols to bring it down safely, using IV meds and constant monitoring. If you don’t have symptoms but your reading is still that high, wait five minutes, recheck, and if it’s still up, call your doctor immediately. Don’t assume it’s a machine error.
Prevention isn’t just about taking pills. It’s about knowing your triggers, tracking your numbers regularly, and having a plan. Keep your meds visible, set phone reminders, and talk to your pharmacist about interactions. Many people don’t realize that a simple cold pill can undo months of control. If you’ve ever had a high reading before, keep a log. Share it with your doctor—not just the numbers, but how you felt. That context is what turns a routine checkup into a lifesaving conversation.
The posts below cover exactly what you need to avoid a high blood pressure emergency—and what to do if it happens. From understanding how medications really work to spotting hidden risks in over-the-counter drugs, these guides give you practical, real-world steps to stay safe. No fluff. No theory. Just what works when your health is on the line.
Severe Hypertensive Crisis from Drug Interactions: What You Need to Know
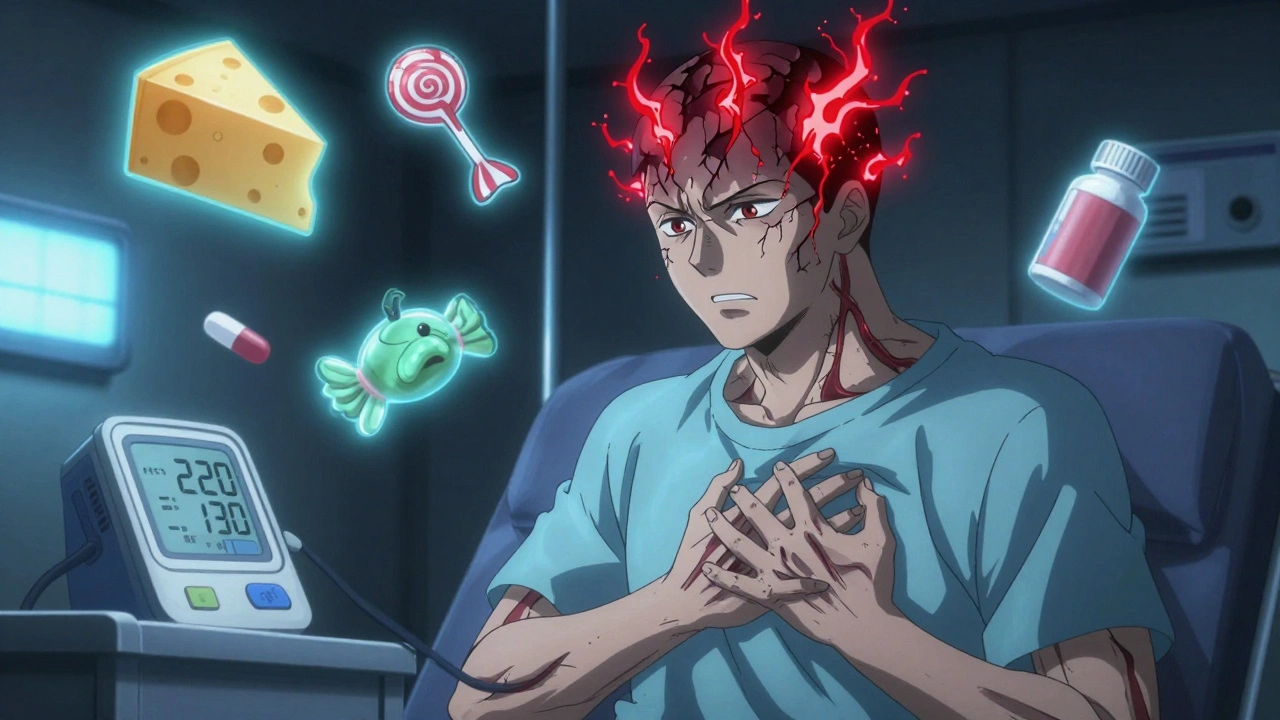
Severe hypertensive crises can be triggered by common drug interactions, including antidepressants, decongestants, and even licorice candy. Learn the hidden risks, warning signs, and how to prevent a life-threatening emergency.
