Exocrine Pancreatic Insufficiency: Causes, Symptoms, and How It Affects Your Digestion
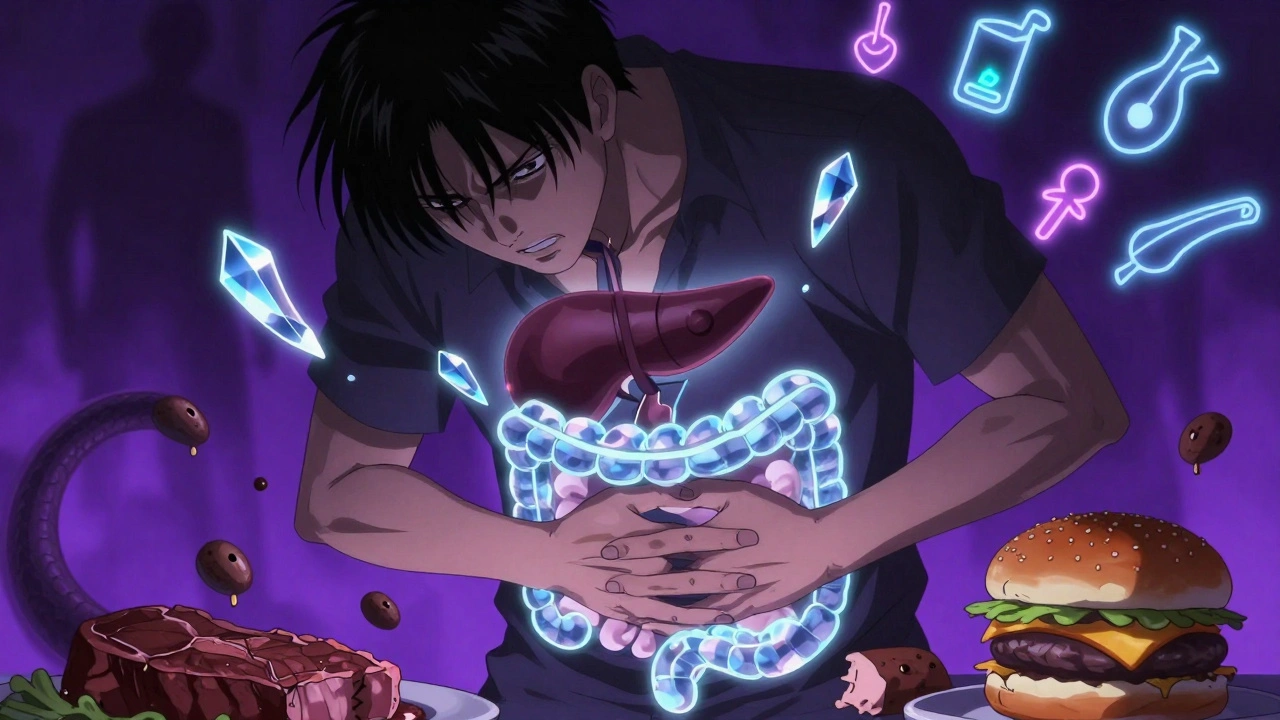
When your exocrine pancreatic insufficiency, a condition where the pancreas fails to produce enough digestive enzymes. It's not just about indigestion—it's your body struggling to break down food so it can absorb nutrients. Also known as EPI, it often gets missed because symptoms like bloating, diarrhea, and weight loss are blamed on other things. Without enough enzymes from the pancreas, fats, proteins, and carbs pass through your gut undigested. That’s why people with EPI often have oily, foul-smelling stools and lose weight even when eating normally.
This isn’t rare. It’s most common after chronic pancreatitis, pancreatic surgery, or in people with cystic fibrosis. But it can also show up with celiac disease, Crohn’s, or even after a gastric bypass. The pancreatic enzyme replacement therapy, prescription pills that replace the enzymes your pancreas can’t make. These are taken with every meal and are the main treatment for EPI. Without them, your body can’t absorb fat-soluble vitamins like A, D, E, and K. That leads to bone loss, night blindness, or easy bruising—problems that seem unrelated but are direct results of poor digestion. Many people live for years with EPI before getting diagnosed because doctors don’t always test for it.
Diagnosing EPI isn’t always straightforward. The fecal elastase-1 test is the most common way—it measures one key enzyme in your stool. Blood tests for vitamin levels can hint at it, but they don’t confirm it. Imaging like CT scans might show pancreatic damage, but they won’t tell you if your enzymes are working. That’s why understanding your symptoms matters more than any single test.
What you eat also plays a role. High-fat meals can make symptoms worse, but cutting fat entirely isn’t the answer—you still need it for vitamins and energy. The goal is balance: smaller meals, consistent enzyme dosing, and tracking what triggers your symptoms. Some people find relief with medium-chain triglyceride oils, which don’t need pancreatic enzymes to break down.
Below are real stories and practical guides from people who’ve dealt with this condition—how they got diagnosed, what treatments helped, and how they learned to eat without fear. You’ll find advice on managing enzyme therapy, spotting hidden signs of deficiency, and avoiding common mistakes that make EPI worse. This isn’t theory. These are the tools and insights that actually work for people living with it every day.
Digestive Enzymes: When Supplements May Help GI Symptoms
Digestive enzyme supplements can help with specific GI issues like lactose intolerance or IBS, but they’re not a cure-all. Prescription enzymes treat EPI; OTC ones offer limited relief. Know when they work - and when to see a doctor.
