By 2023, generic drugs made up 90% of all prescriptions filled in the U.S.-but they only cost 20% of what the country spends on medicine. That sounds like a win. Except millions of patients can’t get them. Insulin, epinephrine, antibiotics, levothyroxine-these aren’t rare or experimental drugs. They’re the ones people rely on every day. And they’re disappearing.
The system was built to save money. Now it’s breaking.
The 1984 Hatch-Waxman Act was supposed to make generics affordable and widely available. It worked. Too well. Generic manufacturers started competing not on quality, but on price. A single tablet might be sold for less than a penny. When a new company enters the market, they undercut the others by a fraction of a cent. The next one drops it again. Soon, no one is making enough to cover costs, let alone invest in better equipment or safer production.Branded drug companies make 70-80% gross margins. Generic manufacturers? Many operate at 15-20%. Some drugs are sold at under 5% profit. That’s not a business. It’s a race to the bottom.
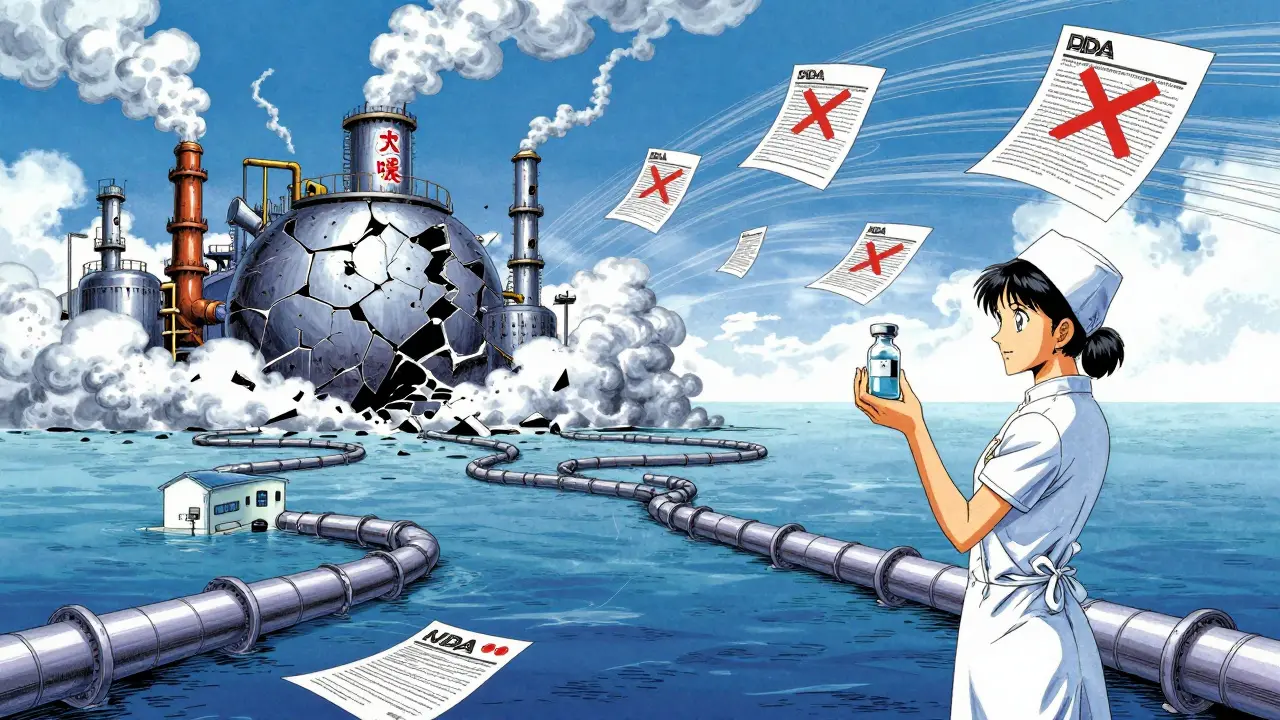
Where your pills are made-and why that matters
Almost 97% of antibiotics, 92% of antivirals, and 83% of the top 100 generic drugs in the U.S. have no active ingredient made here. Instead, they come from factories in India and China. The U.S. used to make 35% of its own active pharmaceutical ingredients (APIs) in 2010. By 2023, that dropped to 14%.It’s not just about distance. It’s about control. One facility makes the API. Another blends it with fillers. A third coats the pill. A fourth packages it. Each step happens in a different country. If one link breaks-say, due to a factory shutdown in China or an export ban in India-the whole chain snaps.
In early 2020, India halted exports of 26 essential medicines, including acetaminophen. That’s the active ingredient in Tylenol. Suddenly, hospitals couldn’t get painkillers or fever reducers. The pandemic didn’t cause the shortage. It exposed it.
Quality control isn’t optional. But it’s expensive.
The FDA inspects foreign facilities less often than U.S. ones. When they do, they find problems. In 2022, Intas Pharmaceuticals in India had its cisplatin-used for cancer treatment-banned from the U.S. market after inspectors found “enormous and systematic quality problems.”U.S. manufacturers keep 95%+ accurate batch records. Some foreign ones? As low as 78%. That gap isn’t just paperwork. It’s safety. A 2023 study found generic drugs made in India had 54% more serious adverse events-including hospitalizations and deaths-than identical drugs made in the U.S. The study didn’t prove cause, but the pattern is too strong to ignore.
Fixing a single FDA inspection violation costs an average of $1.7 million and takes 12 to 18 months. Building a new FDA-approved factory in the U.S. costs $250-500 million. In India? $50-100 million. No wonder companies leave.
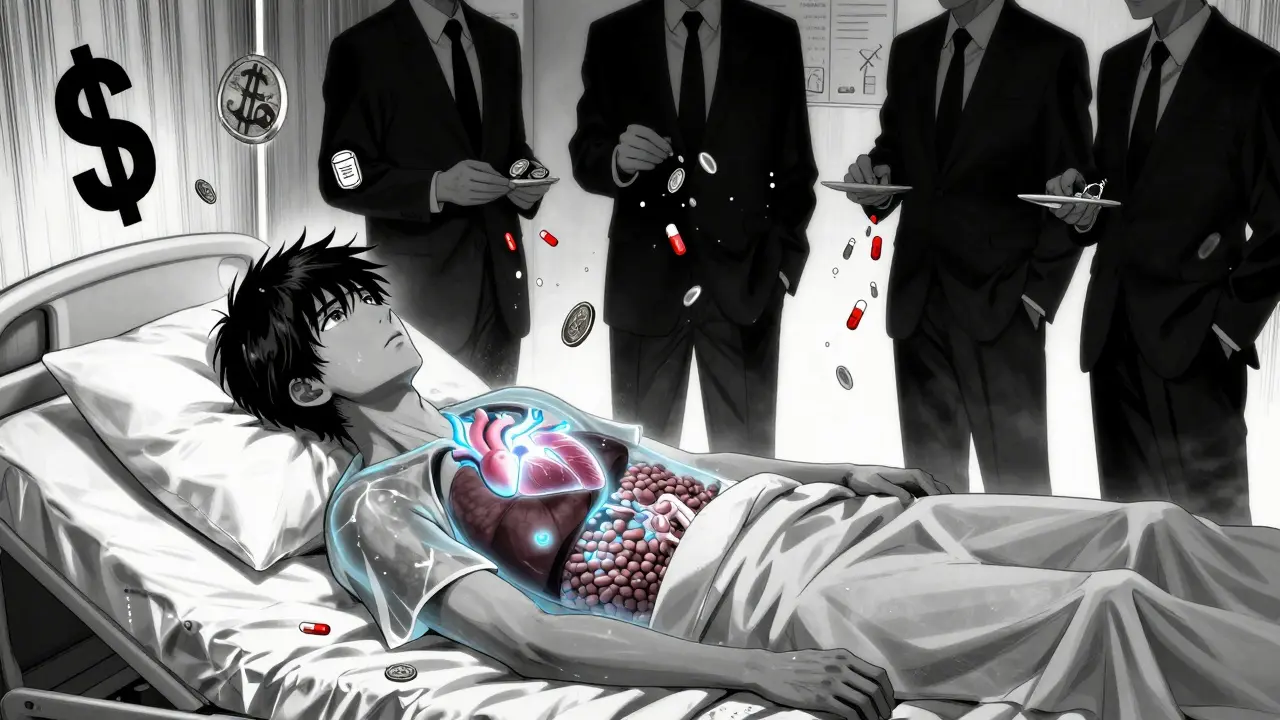
Why no one fixes this
Group purchasing organizations (GPOs) and pharmacy benefit managers (PBMs) control contracts. They pick the cheapest bid-even if it’s from a factory with a history of violations. A hospital might save $50,000 a year on antibiotics by switching to the lowest bidder. But if that supplier shuts down? The hospital can’t just order from someone else. There’s no backup.The FDA can’t force manufacturers to produce more. Their only tool? Calling and asking nicely. In 2023, there were 278 active drug shortages-the highest number since tracking began in 2011. Two-thirds were generics.
Some companies have tried to adapt. A few have invested in continuous manufacturing-technology that monitors quality in real time, reducing errors. But it needs big upfront cash. Only 12 such facilities exist in the U.S. They make less than 3% of all generic drugs.
Who pays the price?
Patients don’t just wait longer. They pay more.When levothyroxine (a thyroid hormone) went short, one nurse practitioner had to switch 89 patients to brand-name versions. Their monthly cost jumped from $10 to $150. Medicare beneficiaries saw heart meds go from $10 to $450 a month.
Pharmacists on Reddit report switching antibiotics for 17 different infections in six months. Cancer patients get delayed treatments. Diabetics ration insulin. Nurses tell stories of patients showing up with symptoms because they couldn’t refill their meds.
It’s not a glitch. It’s a design flaw.
What’s being done-and why it’s not enough
The FDA created a Drug Shortage Task Force. Congress passed the CREATES Act in 2019 to stop branded companies from blocking generic competition. The 2024 federal budget added $80 million for more foreign inspections. That’s a 12% increase. But the number of foreign facilities needing inspection rose by 40%.Bipartisan bills in 2023 proposed tax breaks for U.S.-based API production and national stockpiles of critical drugs. That’s a start. But tax credits won’t fix a market that rewards the lowest bid, no matter the risk.
Some hospitals are bypassing GPOs entirely and negotiating directly with manufacturers. That’s smart. But it only helps big systems. Small clinics and rural pharmacies? They’re still stuck with the lowest bidder.
The future looks bleak-unless we change the rules
By 2027, the number of generic manufacturers serving the U.S. could drop from 127 to 89. That means fewer suppliers, more pressure on the ones left, and more shortages.Experts agree: this isn’t about pandemics or geopolitics. It’s about economics. If you pay less than it costs to make a drug, people stop making it. That’s basic math. The system isn’t broken because of bad actors. It’s broken because the rules reward short-term savings over long-term survival.
There’s no magic fix. But there are choices. We can pay more for generics and keep supply chains stable. Or we can keep chasing pennies-and keep watching essential medicines vanish from shelves.
For now, patients are the ones holding the bag.


Anny Kaettano
January 13, 2026 AT 10:35My grandma takes levothyroxine daily. Last month, her pharmacy gave her a different pill-same name, different shape, different color. She started feeling dizzy. We called the doctor. Turns out the new batch had inconsistent absorption. She’s back on brand now, out-of-pocket. $150/month. She’s on a fixed income. This isn’t just a policy issue. It’s someone’s life.
And don’t tell me ‘just switch to another drug.’ These aren’t choices. These are necessities. We treat generics like commodities, but they’re not. They’re lifelines.
I work in a clinic. We’ve had to ration insulin vials. We’ve had patients cry because they couldn’t refill their antibiotics. We’re not talking about luxury meds. We’re talking about people who can’t afford to die because a factory in India shut down for a ‘quality issue.’
Adam Vella
January 13, 2026 AT 15:26The structural flaw lies not in the manufacturing paradigm per se, but in the misalignment of incentive structures within the pharmaceutical supply chain. The Hatch-Waxman Act, while laudable in intent, created a price-elastic market devoid of margin for quality assurance infrastructure. The concomitant offshoring of active pharmaceutical ingredient (API) production has introduced systemic fragility, compounded by regulatory arbitrage.
When the FDA inspects one facility every 2.7 years on average-compared to 1.4 years domestically-the probability of latent contamination increases exponentially. The 54% higher adverse event rate observed in Indian-manufactured generics is not anomalous; it is the predictable outcome of cost-optimized regulatory compliance.
Moreover, the absence of mandatory batch traceability across international supply chains renders post-market surveillance effectively meaningless. This is not a shortage crisis. It is a governance failure masquerading as market efficiency.
Alan Lin
January 15, 2026 AT 12:56You think this is about money? It’s about dignity. People aren’t asking for luxury. They’re asking not to die because their thyroid med got swapped for a substandard version from a factory that can’t even keep accurate records.
I’ve seen nurses cry because they had to tell a diabetic patient, ‘Sorry, we’re out. Try again next week.’ That’s not healthcare. That’s gambling with lives.
And yes, it’s expensive to build a U.S. facility. But how much does it cost when a patient goes into cardiac arrest because their blood pressure med was underdosed? We’ve already paid that price-hundreds of deaths, thousands of ER visits, families shattered.
It’s time to stop pretending this is a cost problem. It’s a moral one. We need to pay what it takes to make these drugs safely-and we need to do it now. No more ‘we’ll get to it later.’ Later is when someone’s kid dies.
Robin Williams
January 15, 2026 AT 19:23bro. i just found out my azithromycin was made in a factory that got shut down 3 times for ‘contamination.’ i’ve been taking it for my sinus infection. what if i’m just… slowly poisoning myself? like, the pill looks the same. the bottle says the same. but the stuff inside? who knows.
we pay $3 for it. but the real cost? it’s in the hospital bills, the missed work, the grandma who couldn’t get her heart med. we’re all just pretending this is fine.
the system is rigged. and we’re the ones holding the bag. literally.
mike swinchoski
January 16, 2026 AT 14:41People need to stop being so dramatic. It’s just pills. If you can’t afford them, don’t take them. There are natural remedies. Apple cider vinegar cures everything. You want cheap meds? Go to Mexico. Problem solved. Stop blaming corporations. It’s your fault for being lazy and not researching alternatives.
Also, why are you so obsessed with ‘generic’ anyway? Brand name works better. Just pay for it. Grow up.
Trevor Whipple
January 17, 2026 AT 01:31so like… the fda knows all this right? like they’ve seen the reports, the inspection failures, the death stats? then why do they still let these pills in? because they’re cheap? or because they’re scared of pissing off the big pharma lobby? or both?
also-why do we even have gpos? who thought it was a good idea to let a bunch of middlemen pick the cheapest drug for 1000 hospitals? that’s like letting a 12-year-old pick your heart surgery team.
and dont even get me started on india. they make 90% of our antibiotics. but their inspectors? they’re underpaid and overworked. how is that not a disaster waiting to happen?
Lethabo Phalafala
January 17, 2026 AT 14:01I am from South Africa. We have been living this for decades. No insulin. No antibiotics. No antiretrovirals. We watched people die because the global system decided it was ‘too expensive’ to make drugs for us.
Now the U.S. is waking up to the same horror. And guess what? It’s the same factories. The same supply chains. The same greed.
Don’t act like this is new. It’s not. It’s just that now it’s hitting your neighbors, your family, your parents. Before, it was only ‘those people’ in ‘those countries.’
This is colonial medicine. And it’s still alive. And it’s still killing.
Lance Nickie
January 19, 2026 AT 13:06nah bro. the real problem is that people think drugs are a right. they’re not. they’re a product. if you can’t afford it, don’t take it. simple. also, why do you think we have generics? because we’re not all rich. stop crying about pennies.
Damario Brown
January 21, 2026 AT 10:29let me break this down for you like you’re a toddler:
1. generics = low profit
2. low profit = no investment
3. no investment = bad quality
4. bad quality = dead people
5. dead people = no one cares until it’s your mom
the real villain? the PBM that takes 30% of every prescription and pays the manufacturer 2 cents per pill. they’re the ones making millions while nurses cry in the ER.
and don’t even get me started on how the FDA is a toothless tiger. they inspect once every 3 years. meanwhile, factories are cooking up pills in basements with no gloves. this isn’t a crisis. it’s a crime scene.
sam abas
January 21, 2026 AT 19:17Look, I’ve read the FDA reports. I’ve cross-referenced the 2023 shortage data with the 2022 inspection logs. The correlation between inspection violations and drug shortages is statistically significant at p < 0.001. But here’s the thing: the real issue isn’t the factories. It’s the lack of vertical integration. The entire supply chain is a Rube Goldberg machine designed by economists who’ve never held a pill in their hand.
What if we nationalized API production? What if we mandated minimum profit margins for essential generics? What if we created a public-private consortium to fund continuous manufacturing tech? The solutions exist. But they require political will-and that’s the real bottleneck.
Also, why are we still using batch records? We have real-time sensors now. We could monitor every gram of active ingredient. But no one wants to spend the $200 million to upgrade. Because the next bid is 0.003 cents cheaper.
It’s not broken. It’s designed this way. And we’re all complicit.
Clay .Haeber
January 22, 2026 AT 04:38Oh wow. A 17-page essay on how capitalism failed. Shocking. Next you’ll tell me water is wet and gravity exists.
So let me get this straight: we pay less for drugs… and now people are mad? Who knew? Maybe if you spent less time on Reddit and more time working overtime, you could afford the $150 thyroid med.
Also, why are you blaming India? They’re just doing what we asked them to do: make it cheap. We didn’t say ‘make it safe.’ We said ‘make it cheap.’ Guess what? They listened.
Stop pretending this is a moral issue. It’s a you-problem. You wanted cheap. Now you’re getting what you paid for. Welcome to capitalism. It’s not a bug. It’s a feature.
Priyanka Kumari
January 22, 2026 AT 18:15As someone from India, I want to say this with deep respect: many of our manufacturers are hardworking, ethical, and deeply committed to global health. But they are trapped in a system where the lowest bid wins-and they are forced to cut corners just to survive.
I’ve visited factories in Gujarat and Hyderabad. The workers are skilled. The machines are old. The inspectors are few. The pressure is immense.
But here’s the truth: we don’t want to be the world’s pharmacy because we’re cheap. We want to be the world’s pharmacy because we’re capable. And we need fair pricing-not exploitation-to do it right.
Let’s not villainize Indian workers or Chinese engineers. Let’s fix the system that makes them choose between safety and survival. We’re all in this together.
Alan Lin
January 24, 2026 AT 08:34Replying to @6805: You’re right. The workers aren’t the enemy. The system is.
And here’s what no one says: if we paid $0.05 more per pill for insulin, we could double the number of FDA inspections in India. We could fund modernization. We could hire more inspectors. We could build U.S. backup capacity.
That’s $50 million a year. The U.S. spends $1.2 billion a year on generic drugs. We’re talking about 0.004% more.
But we’d rather let people die than pay a nickel more.
That’s not economics. That’s cruelty dressed up as efficiency.