When you find an old pill bottle in the back of your medicine cabinet, the expiration date staring back at you isn’t just a suggestion-it’s a legal and scientific boundary set by the manufacturer. But what does that date actually tell you? Is that medicine still safe? Will it even work? Many people assume expired meds are dangerous, while others think they’re fine if they look okay. The truth is somewhere in between-and it’s more complicated than you think.
What the Expiration Date Actually Means
The expiration date on your medication isn’t when the drug turns toxic. It’s the last day the manufacturer guarantees the medicine will work exactly as intended-full strength, pure, and safe-under proper storage conditions. This date comes from rigorous testing required by the U.S. Food and Drug Administration since 1979. Companies must prove their drugs stay above 90% potency and stay within safe impurity limits through stability tests that simulate real-world conditions: heat, humidity, and light.
Most expiration dates are set between 12 to 60 months after production. But here’s the catch: those tests are done in controlled labs. If you store your pills in a steamy bathroom or a hot car, the real shelf life shrinks fast. The FDA says the date is absolute. But research tells a different story.
What Happens When Medications Expire?
Most solid medications-like tablets and capsules-don’t suddenly become harmful after their expiration date. Instead, they slowly lose potency. A landmark study by the U.S. military’s Shelf Life Extension Program (SLEP), which tested over 3,000 lots of 122 drugs between 1985 and 2006, found that 88% of them were still effective 15 years past their printed date. Some, like ciprofloxacin and amoxicillin, retained over 90% potency even after a decade or more.
That doesn’t mean you should stockpile antibiotics for the next pandemic. But it does mean that for many common drugs-like ibuprofen, acetaminophen, or blood pressure pills stored in a cool, dry place-the expiration date is more of a conservative estimate than a hard cutoff.
The Real Danger: When Expired Drugs Can Hurt You
Not all meds are created equal. Some drugs degrade quickly-and dangerously-after expiration. These aren’t just less effective. They can fail you when you need them most.
- Nitroglycerin: Used for heart attacks, it loses half its strength within months after opening-even before the expiration date. Taking expired nitroglycerin during chest pain could mean the difference between life and death.
- Insulin: Once opened, insulin breaks down at 1.5-2.5% per month if not refrigerated. A weakened dose won’t control blood sugar, leading to dangerous highs or lows.
- Liquid antibiotics: Amoxicillin-clavulanate suspension becomes ineffective after 14 days, no matter what the bottle says. Using it past that point can lead to antibiotic resistance or untreated infections.
- Epinephrine auto-injectors (EpiPens): These save lives during allergic reactions. After expiration, they lose 15-20% potency each year. In an emergency, that drop could mean an incomplete dose.
- Warfarin: This blood thinner has a narrow safety window. Expired versions can cause unpredictable clotting or bleeding risks.
The Institute for Safe Medication Practices calls these high-risk medications. If you’re using one of these for a life-sustaining condition, don’t gamble with expiration dates.

Storage Matters More Than You Think
Your medicine’s real lifespan depends more on how you store it than what’s printed on the label.
Heat and moisture are the biggest enemies. Bathrooms are the worst place to keep meds-the humidity from showers can reach 85%, accelerating degradation. A hot car in summer? Even worse. The European Medicines Agency says storing drugs at 30°C instead of 25°C can cut their shelf life by 40-60%.
Keep pills in their original bottles with the child-resistant cap tightly closed. Store them in a cool, dry place-like a bedroom drawer, not the kitchen cabinet above the stove. Avoid clear plastic containers unless they’re light-blocking. Sunlight breaks down some medications faster than you’d expect.
If your pills look weird-discolored, cracked, smelly, or sticky-throw them out. That’s not just a precaution. It’s a warning sign the chemical structure has changed.
When It’s Okay to Use an Expired Medicine
There’s no universal rule, but experts agree on a few practical guidelines:
- Low-risk meds (like statins, antidepressants, or allergy pills) stored properly may still work years past expiration. If you’re out of refills and can’t get a new prescription, using one of these briefly isn’t likely to cause harm.
- Never use expired meds for serious conditions: infections, heart disease, seizures, or asthma. The risk of treatment failure is too high.
- Emergency drugs like EpiPens, nitroglycerin, or seizure meds should always be replaced on schedule. There’s no safe gray area here.
Pharmacists at Johns Hopkins and other major hospitals have noted that during drug shortages, some expired, stable medications may be used temporarily under medical supervision. But that’s not something you should do on your own.
What to Do With Expired Medications
Don’t flush them unless they’re on the FDA’s Flush List (like fentanyl patches or oxycodone tablets). Flushing pollutes waterways. Don’t toss them in the trash either-someone might dig them out.
The safest option? Use a drug take-back program. In 2023, U.S. law enforcement collected over 900,000 pounds of unused meds during National Prescription Drug Take-Back Days. These events happen twice a year, and there are over 5,800 drop-off sites nationwide.
If you can’t wait for a take-back day, mix pills with kitty litter or coffee grounds, seal them in a plastic bag, and throw them in the trash. It’s not perfect, but it makes them unappealing and harder to misuse.
What’s Changing in the Future
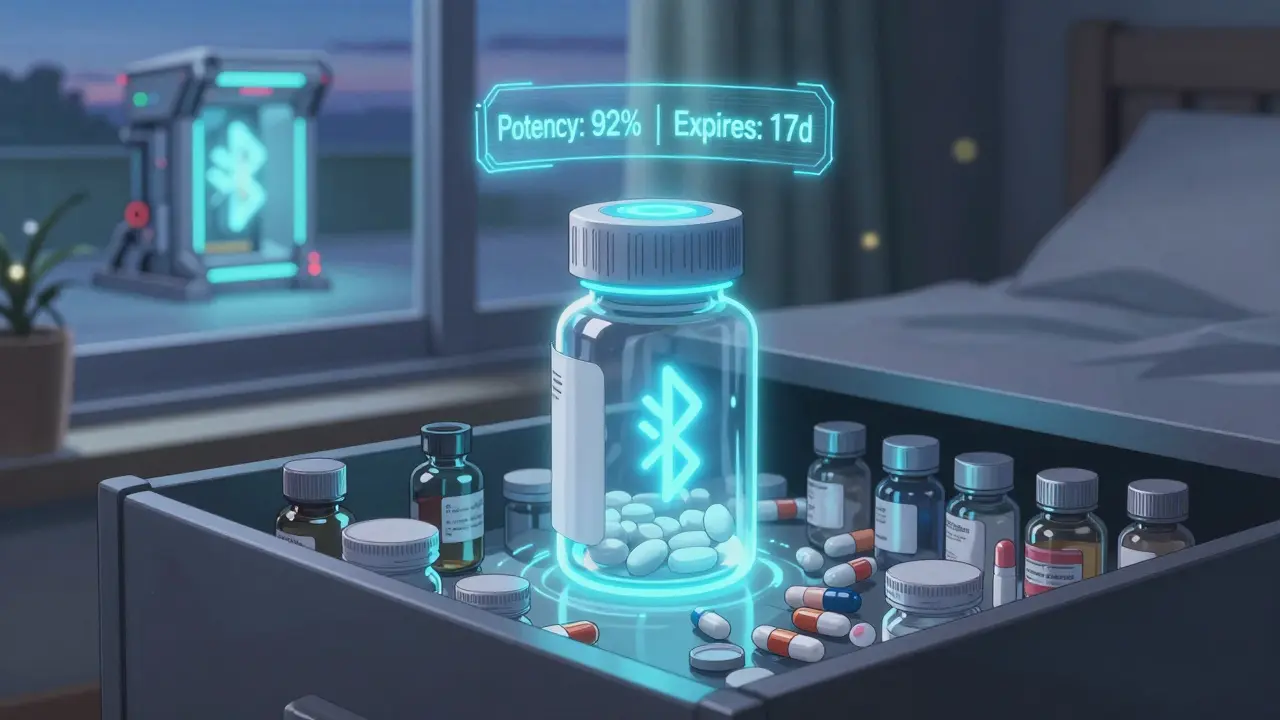
The system is starting to evolve. The FDA is testing smart packaging with Bluetooth sensors that track real-time temperature and humidity. These devices could update expiration dates based on actual conditions-so your insulin might say "expires in 30 days" instead of "expires in 2024" if it’s been stored right.
Researchers at the University of Utah are building AI models that predict how much potency remains in a drug based on its storage history. Early results show 89.7% accuracy for common medications.
And the economic pressure is growing. The U.S. throws away $765 billion in expired meds every year. The military saves $1.2 billion annually by extending expiration dates on stockpiled drugs. More countries are starting to allow expiration date extensions for emergency supplies. The question isn’t whether we’ll change how we handle expired meds-it’s how fast.
Bottom Line: Use Judgment, Not Fear
Expired medications aren’t all dangerous. But they’re not all safe, either. The key is knowing which ones matter and how you’ve stored them.
If it’s a daily pill for high blood pressure, stored in a cool drawer, and it’s six months past expiration? Probably fine for a few more days while you wait for your refill.
If it’s your EpiPen, your insulin, or your child’s antibiotics? Don’t risk it. Replace it.
When in doubt, talk to your pharmacist. They’re trained to assess expiration risks and can tell you whether a drug is still usable-or if you need a new prescription. Your safety isn’t about following a date on a bottle. It’s about making smart, informed choices.
Is it dangerous to take expired medication?
For most solid medications stored properly, taking them past the expiration date isn’t dangerous-it just means they might not work as well. But for certain drugs like insulin, nitroglycerin, epinephrine, or liquid antibiotics, expired versions can be ineffective or even life-threatening. Always check the type of medication before deciding.
Do expiration dates apply to over-the-counter drugs too?
Yes. All prescription and over-the-counter medications sold in the U.S. must have an expiration date. The same rules apply: potency degrades over time, and storage conditions matter. Even common pain relievers like ibuprofen or aspirin lose strength after several years, especially if exposed to heat or moisture.
Can I use expired antibiotics?
Avoid it. Expired antibiotics may not kill all the bacteria, which can lead to antibiotic resistance or a worsening infection. Solid forms like pills might retain some potency, but liquid suspensions become useless after 14 days. Never use expired antibiotics for a new infection without a doctor’s advice.
How should I store medications to make them last longer?
Keep them in their original containers, tightly sealed, in a cool, dry place away from sunlight. A bedroom drawer is better than a bathroom cabinet. Avoid temperatures above 25°C (77°F) and humidity over 60%. Never store pills in your car or near the stove.
What if I can’t afford to replace my expired medication?
Talk to your pharmacist or doctor. Many pharmacies offer low-cost generic alternatives or patient assistance programs. For life-sustaining medications, some manufacturers provide free or discounted replacements if you explain your situation. Never skip doses or use expired drugs for critical conditions just because of cost.
Are there any countries that allow expired medications to be used?
Yes. Over 60 countries allow expiration date extensions for emergency medical stockpiles, especially for military or disaster response. But only 12% of nations permit consumers to use expired meds under any circumstances. In the U.S., it’s not officially allowed-even if research shows many drugs remain effective.


Lydia H.
January 18, 2026 AT 17:59So many people panic about expiration dates like they’re ticking time bombs, but honestly? Most pills are fine if stored right. I’ve got ibuprofen from 2020 in my drawer and it still works like a charm. No need to toss everything just because the label says so.
Aman Kumar
January 18, 2026 AT 19:02Let’s be clear: the pharmaceutical industry has vested interests in maintaining artificial expiration windows. The SLEP data is irrefutable-88% of pharmaceuticals retain therapeutic efficacy beyond their labeled shelf life. This is not anecdotal; it’s evidence-based pharmacokinetics. To discard perfectly viable medication due to arbitrary regulatory compliance is economically irresponsible and ethically indefensible.
Moreover, the FDA’s stance is rooted in liability mitigation, not clinical necessity. The real crisis is not expired meds-it’s the systemic failure to provide affordable access to life-sustaining drugs. People are choosing between rent and refills. Yet we’re lectured about discarding perfectly usable tablets? Absurd.
Let’s reframe this: expiration dates are not safety thresholds-they are commercial constructs. We need policy reform, not fear-mongering.
Jake Rudin
January 19, 2026 AT 18:41Interesting… but… I mean… what if… you’ve got a bottle of, like, amoxicillin… from… 2018… and… you’re… in… the woods… and… your kid… is… sick… and… you’ve… got… no… other… options…?
Like… do you… just… let… them… suffer…?
Or… do… you… take… a… chance…?
Because… the… science… says… it’s… probably… fine… but… the… label… says… DON’T… and… your… brain… is… screaming… ‘WHAT IF IT’S TOXIC?!’
So… yeah… I… guess… I’d… take… it… but… I’d… feel… guilty… about… it…
Astha Jain
January 21, 2026 AT 09:32OMG i just found my grandmas epipen from 2019 and it was still in the box but like… i mean… it’s expired so i just tossed it?? but now i’m like… wait… was that dumb??
Phil Hillson
January 23, 2026 AT 07:37Ugh another one of these articles that makes you feel guilty for not being a pharmacist
Look I have a drawer full of expired meds and I’m not going to throw them out just because some bureaucrat decided that 2024 is the magic number
Also who stores meds in the bathroom? That’s not a question that needs answering
Just take the damn pill if it looks fine and stop overthinking it
Josh Kenna
January 23, 2026 AT 14:57I get what you’re saying but I’m scared to use anything expired after my aunt took some old antibiotics and got sepsis. I know it’s rare but… what if it’s me? I’d rather spend $15 on a new prescription than risk it. My pharmacist told me if it’s not life-saving and stored well, it’s probably fine-but I still panic. I think I’m just wired that way.
Erwin Kodiat
January 25, 2026 AT 14:41I lived in Thailand for a year and saw pharmacies sell meds past expiration all the time-no one freaked out. People just checked the color and smell. If it looked and felt normal, they used it. I started doing the same. My headache pills from 2021 still work. Maybe the fear is more cultural than scientific?
Valerie DeLoach
January 25, 2026 AT 22:24There’s a profound irony here: we live in a world where we’re told to be scientifically literate, yet we’re conditioned to treat expiration dates as divine law-ignoring the very data that shows their conservatism. The real danger isn’t the expired pill-it’s the erosion of critical thinking, replaced by blind compliance with institutional labels.
Pharmacists are trained to assess risk, not just read dates. Why don’t we empower patients to do the same? Education, not fear, should guide our decisions. And yes-storage matters more than the printed date. A pill in a cool, dry drawer is far more stable than one in a steamy bathroom.
For high-risk medications, caution is non-negotiable. For others? Let’s stop treating patients like children who can’t handle nuance.
Christi Steinbeck
January 26, 2026 AT 12:51STOP WASTING MONEY ON MEDS YOU DON’T NEED. If you’ve got ibuprofen from 2020 and it’s not discolored? USE IT. Your wallet will thank you. Your body won’t care. Stop letting corporations profit off your fear. Replace the life-saving stuff, sure-but don’t flush your savings down the toilet because of a date.