When a drug has a narrow therapeutic index, even a tiny change in dose can mean the difference between healing and harm. Theophylline is one of those drugs. Used for decades to treat asthma and COPD, it’s cheap, effective, and still in use - but only if you monitor it closely. Without regular blood tests, theophylline can slip from life-saving to life-threatening in days, sometimes hours. This isn’t theoretical. People end up in the ER because their levels crept up after starting an antibiotic, or dropped after they quit smoking. And it’s not just about the dose - it’s about what’s happening inside your body.
What Makes Theophylline So Dangerous?
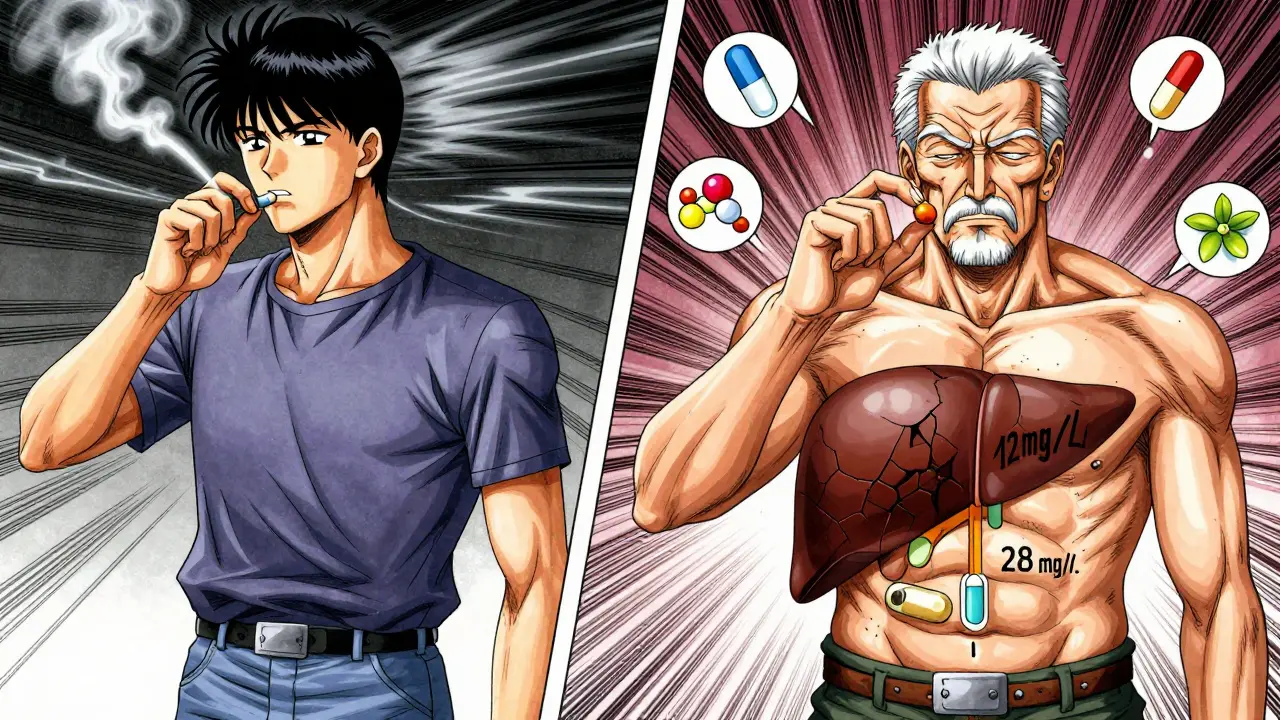
Theophylline works by relaxing airway muscles and reducing lung inflammation. Its sweet spot? A blood concentration between 10 and 20 mg/L. Below 10, it barely helps. Above 20, you’re in danger. At 25 mg/L or higher, the risk of seizures, irregular heartbeats, and even death jumps sharply. That’s a tiny window - about the width of a pencil eraser on a scale that spans from safe to deadly.
What makes this worse is how unpredictable the drug is. Two people taking the same 400 mg dose can have wildly different blood levels. One might stay at 12 mg/L. The other hits 28 mg/L - and ends up in the hospital. Why? Because theophylline is metabolized by the liver, and that process varies wildly between people.
Why Your Body Changes How It Handles Theophylline
Your liver doesn’t always work the same way. Things like age, illness, or even what you ate yesterday can shift how fast your body clears the drug.
- Smokers clear theophylline 50-70% faster. Quit smoking, and your levels can spike within days.
- Pregnant women, especially in the third trimester, metabolize it 30-50% slower.
- People over 60, or those with heart or liver failure, break it down much slower - sometimes by half.
- Alcohol? It can drop your levels. Coffee? It can raise them.
And then there are the drugs. Common antibiotics like erythromycin and ciprofloxacin can boost theophylline levels by 50-100%. That’s not a minor interaction - it’s a red alert. On the flip side, drugs like carbamazepine or St. John’s Wort can slash levels by 30-60%, making your asthma flare up again. Many patients don’t even know they’re taking something that interferes. A simple cold medicine or herbal supplement can be the trigger.
When and How Often Should You Get Tested?
Testing isn’t optional - it’s the only way to know if the drug is working safely. But timing matters.
For immediate-release tablets, blood should be drawn right before your next dose - that’s the trough level, the lowest point. For extended-release versions, test 4 to 6 hours after taking it. Waiting too long or too short gives you the wrong number.
Here’s the real-world schedule:
- Start monitoring 5 days after beginning treatment, or 3 days after any dose change - that’s when steady levels settle in.
- Stable patients: every 6-12 months.
- Over 60? Every 3-6 months.
- Heart failure, liver disease? Every 1-3 months.
- Pregnant? Monthly during the second and third trimesters.
And if you start a new medication, quit smoking, get sick, or feel weird - get tested immediately. Nausea, tremors, rapid heartbeat, or trouble sleeping? Those aren’t side effects you should tolerate. They’re warning signs.
What Else Should Doctors Watch For?
It’s not just about theophylline levels. You need to look at the whole picture.
- Heart rate over 100 bpm? Could be early toxicity.
- Low potassium? Common if you’re also on albuterol or steroids. Low potassium makes arrhythmias more likely.
- Headache, insomnia, anxiety? Those are CNS signs - often missed until it’s too late.
- IV theophylline? Never mix it with dextrose. It can cause clumping or even destroy red blood cells.
One 2023 case report showed a 68-year-old man with COPD developing life-threatening ventricular tachycardia after starting ciprofloxacin. His theophylline level jumped from 14 mg/L to 28 mg/L in 72 hours. He survived - but barely. That kind of story isn’t rare.
What Happens When Monitoring Is Ignored?
Studies show that 15% of theophylline-related emergencies happen because doctors didn’t adjust for liver problems. Another 22% come from unmonitored drug interactions - mostly with antibiotics.
One hospital that implemented a strict monitoring protocol cut adverse events by 78% and improved asthma control by 35% in just 18 months. That’s not a small win. That’s life-changing.
On the flip side, patient surveys show that 68% of long-term users find blood tests annoying - but 82% say their breathing is better when levels are in range. The inconvenience is real. But so is the risk.

Is Theophylline Still Worth It?
It’s not the first-line drug anymore. Inhaled steroids and long-acting bronchodilators are safer and easier to use. But for some people - especially those with severe, hard-to-control asthma or in places where biologics cost $400 a month - theophylline is still a lifeline. It costs $15-$30 a month. That’s not a luxury. It’s accessible care.
Some argue that low doses (200 mg/day) are safe enough to skip monitoring. But the European Respiratory Society and the American College of Chest Physicians say no. Even low doses can be dangerous if metabolism changes. You can’t assume safety just because the dose is small.
The Future: Faster Testing?
Three companies are testing handheld devices that could give theophylline results in under five minutes. Imagine getting your level checked at the pharmacy, or even at home. That could change everything - especially for elderly patients who struggle with clinic visits.
But until those tools are proven and widely available, the standard hasn’t changed: blood tests are non-negotiable. The American College of Chest Physicians says it plainly: “Traditional serum concentration monitoring remains the standard of care.”
And the numbers don’t lie. Between 2020 and 2023, theophylline toxicity cases reported to U.S. poison control centers rose 23% per year. Most were in older adults with undiagnosed liver or kidney problems. They weren’t overdosing. They were just getting older - and no one checked their levels.
Bottom Line: No Monitoring, No Safety
Theophylline isn’t a drug you take and forget. It’s a tool that demands respect. It’s powerful. It’s cheap. And it’s unforgiving. If you’re on it, you need regular blood tests. Not because you’re being paranoid - because the science says so. Your liver changes. Your meds change. Your body changes. If you don’t track it, you’re gambling with your health.
There’s no substitute for knowing your level. No app. No symptom checklist. No guesswork. Just a tube of blood and a lab result. That’s the only way to make sure you’re getting the benefit - without the risk.
How often should theophylline levels be checked?
For new patients or after a dose change, check after 5 days (or 3 days for extended-release). Stable adults: every 6-12 months. Older adults, heart or liver patients: every 1-3 months. Pregnant women: monthly in the second and third trimesters. Always test if you start a new medication, quit smoking, or have new symptoms like nausea or palpitations.
What happens if theophylline levels are too high?
Levels above 20 mg/L increase risk of side effects. Above 25 mg/L, toxicity becomes likely: nausea, vomiting, tremors, rapid heartbeat. At 30 mg/L or higher, seizures and life-threatening arrhythmias can occur. The mortality rate in severe cases can reach 10%. This isn’t a minor issue - it’s an emergency.
Can I take theophylline without blood tests?
No. Even low doses require monitoring. The drug’s metabolism varies too much between people due to age, liver function, smoking, and other medications. A 2024 study suggested low doses might be safer, but major medical societies like the European Respiratory Society and American College of Chest Physicians still require monitoring for all patients. There is no safe way to skip it.
Which drugs interact with theophylline?
Many. Antibiotics like erythromycin, clarithromycin, and ciprofloxacin can raise levels by 50-100%. Cimetidine and allopurinol do the same. On the other hand, carbamazepine, rifampin, and St. John’s Wort can lower levels by 30-60%. Even caffeine and alcohol affect it. Always tell your doctor what you’re taking - including OTC meds and supplements.
Why is theophylline still used if it’s so risky?
It’s one of the few affordable options for severe asthma and COPD. Biologics cost $200-$400 a month. Theophylline costs $15-$30. For patients without good insurance or in low-resource areas, it’s still a vital tool - if monitored properly. Its anti-inflammatory effects also help in severe asthma where steroids aren’t enough. The risk is real, but so is the benefit - when managed correctly.
Do I need to stop theophylline if I get sick?
Not necessarily, but you should get tested. Illness - especially fever, pneumonia, or liver stress - can slow how fast your body clears the drug. This can cause levels to rise dangerously. Don’t stop it on your own. Talk to your doctor, get a blood test, and adjust only under medical guidance.
What symptoms should make me call my doctor right away?
Call immediately if you have nausea/vomiting that won’t stop, tremors, rapid or irregular heartbeat, confusion, seizures, or chest pain. These are signs of toxicity. Don’t wait for your next appointment. Go to urgent care or the ER. Theophylline toxicity can progress quickly and is life-threatening.
Can I monitor theophylline at home?
Not yet. While handheld devices are in development and undergoing clinical trials, no home test is approved or widely available. Blood tests through a lab are still the only reliable method. Don’t rely on apps, symptoms, or guesswork - they’re not accurate enough.


Janette Martens
December 30, 2025 AT 13:43Russell Thomas
January 1, 2026 AT 09:55Joe Kwon
January 1, 2026 AT 12:29Nicole K.
January 2, 2026 AT 02:23Amy Cannon
January 4, 2026 AT 00:31Himanshu Singh
January 4, 2026 AT 17:12Alex Ronald
January 5, 2026 AT 02:21Teresa Rodriguez leon
January 6, 2026 AT 11:07Marie-Pierre Gonzalez
January 8, 2026 AT 03:06