Understanding Pancreatic Cancer and Cyclophosphamide
Pancreatic cancer is a highly aggressive and difficult-to-treat type of cancer that affects the pancreas, an organ in the abdomen responsible for producing insulin and other hormones. Pancreatic cancer is often diagnosed at advanced stages, which makes treatment more challenging. In this article, we will discuss the use of cyclophosphamide, a chemotherapy drug, in the treatment of pancreatic cancer.
Cyclophosphamide is an alkylating agent that interferes with the DNA of cancer cells, preventing them from dividing and growing. It has been used for many years in the treatment of various types of cancer, including breast cancer, lymphoma, and leukemia. In recent years, researchers have been exploring the potential of cyclophosphamide in treating pancreatic cancer, with some promising results.
How Cyclophosphamide Works Against Pancreatic Cancer
As mentioned earlier, cyclophosphamide works by interfering with the DNA of cancer cells, ultimately leading to cell death. Specifically, it forms highly reactive molecules called alkyl groups, which bind to the DNA strands and cause breaks in the double helix structure. This prevents the cancer cells from dividing and eventually leads to their death.
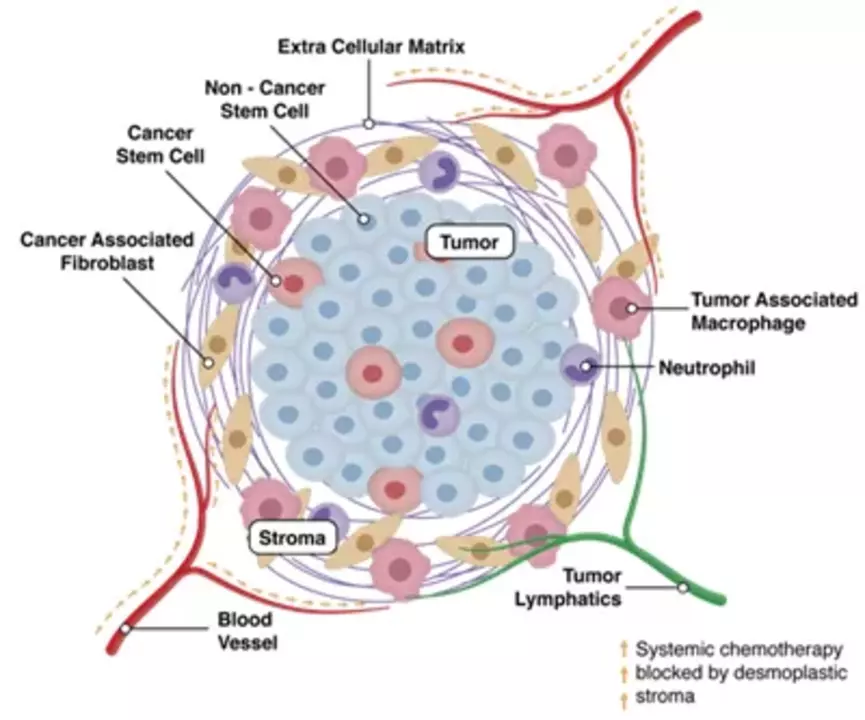
In pancreatic cancer, cyclophosphamide has been shown to have a cytotoxic effect on both the cancer cells and the tumor microenvironment, which is the environment surrounding the tumor that supports its growth. By targeting both the tumor cells and their supportive environment, cyclophosphamide may help to slow down the growth of pancreatic cancer and improve treatment outcomes.
Combination Therapy with Cyclophosphamide
One of the main strategies in treating pancreatic cancer is using a combination of different therapies to target multiple aspects of the disease. Cyclophosphamide is often combined with other chemotherapy drugs, such as gemcitabine or 5-fluorouracil, to enhance its effectiveness against pancreatic cancer. This combination therapy approach can help to increase the chances of a favorable response and delay disease progression.
In addition to being combined with other chemotherapy drugs, cyclophosphamide has also been studied in combination with targeted therapies, such as tyrosine kinase inhibitors, and immunotherapies, which help to stimulate the immune system to attack cancer cells. These combinations are still being investigated in clinical trials, but they show promise for improving the treatment of pancreatic cancer.
Side Effects of Cyclophosphamide in Pancreatic Cancer Treatment
Like any chemotherapy drug, cyclophosphamide can cause side effects in patients undergoing treatment for pancreatic cancer. Some common side effects include nausea, vomiting, hair loss, fatigue, and a decrease in blood cell counts, which can lead to an increased risk of infections, anemia, or bleeding. It is important to discuss these side effects with your healthcare team and to report any new or worsening symptoms during treatment.
In some cases, the dose of cyclophosphamide may need to be adjusted or treatment may need to be delayed to manage these side effects. Supportive care, such as medications to control nausea or prevent infections, can also help to minimize the impact of side effects on a patient's quality of life during treatment.
Understanding the Potential Benefits and Limitations of Cyclophosphamide
While cyclophosphamide has shown promise in the treatment of pancreatic cancer, it is important to understand that it is not a cure for the disease. The goal of treatment with cyclophosphamide and other chemotherapy drugs is to slow down the growth of the cancer, relieve symptoms, and improve a patient's quality of life.
It is also important to recognize that not all patients with pancreatic cancer will respond to cyclophosphamide or combination therapy. Factors such as the stage of the disease, the specific genetic makeup of the tumor, and the overall health of the patient can all influence treatment outcomes. Therefore, it is crucial to discuss your individual situation and treatment options with your healthcare team.
Future Directions in Pancreatic Cancer Treatment and the Role of Cyclophosphamide
While the use of cyclophosphamide in the treatment of pancreatic cancer shows promise, there is still much to learn about the optimal ways to use this drug and to combine it with other therapies. Ongoing research and clinical trials are crucial to improving our understanding of how to best treat pancreatic cancer and to develop new, more effective therapies.
As a patient or caregiver, it is important to stay informed about the latest research and advances in pancreatic cancer treatment. This can help you to advocate for the best possible care and make informed decisions about your treatment options. By working together with your healthcare team and staying informed, we can continue to make progress in the fight against pancreatic cancer.

Dylan Mitchell
May 6, 2023 AT 03:53This cyclo thing is like totally a game‑changer!
Elle Trent
May 6, 2023 AT 05:00Alright, let’s cut to the chase – the whole cyclophosphamide combo feels like another buzzword‑filled regimen that doctors love to toss around. It’s got the typical chemo‑cocktail vibe, with gemcitabine and 5‑FU tagging along. Sure, the micro‑environment targeting sounds fancy, but at the end of the day, you’re still looking at the same old side‑effect profile.
Jessica Gentle
May 6, 2023 AT 06:06Happy to dive a bit deeper into how cyclophosphamide fits into the broader pancreatic cancer treatment landscape. First off, it’s an alkylating agent that creates cross‑links in DNA, effectively halting cell division in rapidly proliferating tumor cells. This mechanism isn’t new, but its role in modulating the tumor microenvironment is gaining attention – the drug can disrupt stromal support and potentially enhance immune infiltration.
When paired with gemcitabine, the synergy appears to stem from complementary mechanisms: gemcitabine hampers DNA synthesis while cyclophosphamide adds a layer of DNA damage that can overwhelm repair pathways. Some early phase trials have reported modest improvements in progression‑free survival, though the data are still emerging.
It’s also worth noting that dosing schedules matter. Metronomic (low‑dose, frequent) administration of cyclophosphamide has been explored to reduce toxicity while maintaining anti‑angiogenic effects. Patients tend to tolerate this approach better, experiencing fewer severe neutropenia episodes.
From a side‑effect standpoint, you’ll still see the classic nausea, alopecia, and marrow suppression, but proactive supportive care – anti‑emetics, growth factors, and close monitoring – can mitigate many of these issues. Individual patient factors, such as baseline renal function and performance status, should guide dose adjustments.
Looking ahead, the most exciting developments involve combination strategies with immune checkpoint inhibitors. By weakening the tumor’s defensive stroma, cyclophosphamide may prime the immune system for a more robust response to drugs like pembrolizumab. Ongoing trials are testing this hypothesis, and early signals are encouraging.
In practice, the decision to incorporate cyclophosphamide should be individualized. Discuss with the oncology team about the potential benefits, the expected side‑effect profile, and any clinical trial options that might be available. Staying informed and proactive is key to optimizing outcomes.
Samson Tobias
May 6, 2023 AT 07:13That’s a solid breakdown, and I’d add that patient morale plays a huge role in tolerating any regimen. Encouraging small victories – like a good day without nausea – can boost adherence. Also, keep the line open with your care team for rapid tweaks; sometimes a slight schedule shift makes a world of difference.
Alan Larkin
May 6, 2023 AT 08:20Just a quick note: the pharmacokinetics of cyclophosphamide indicate a need for adequate hydration to prevent urotoxicity. Also, don’t forget the role of mesna when dosing high‑intensity regimens 😊.