Understanding Parkinson's Disease
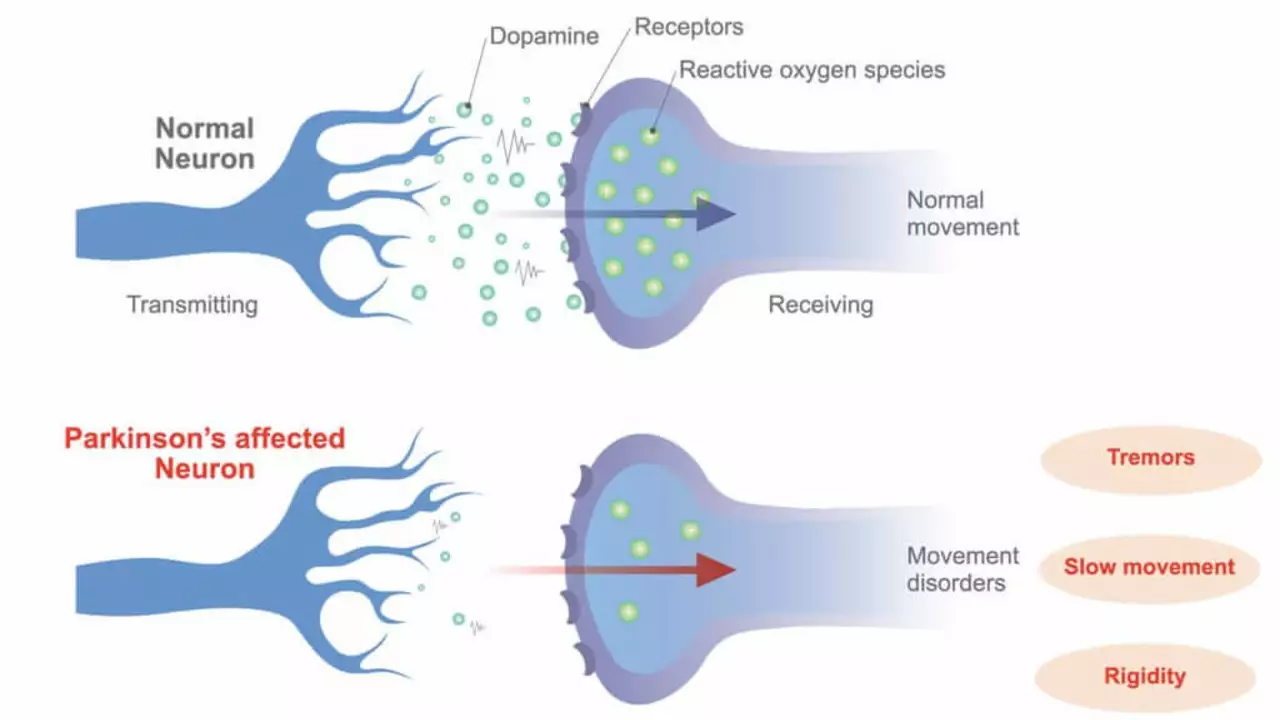
Parkinson’s disease is a neurodegenerative disorder that affects predominantly dopamine-producing neurons in a specific area of the brain. Symptoms generally develop slowly over years, and include tremors, bradykinesia (slowness of movement), limb rigidity, and balance problems. Although there is currently no cure for Parkinson's disease, several types of medications can provide dramatic relief from the symptoms.
Introduction to Rasagiline
Rasagiline is one such medication. It belongs to a class of drugs known as monoamine oxidase inhibitors (MAOIs) that increase the levels of certain chemicals in the brain. Rasagiline is used to treat symptoms of Parkinson's disease and can be used alone or with other drugs. It is used to improve quality of life, functionality, and the time between the start of symptoms and the need for other medications.
Working Mechanism of Rasagiline
Rasagiline works by increasing the levels of certain chemicals in the brain. It helps to improve symptoms of Parkinson's disease such as stiffness, shakes, and difficulty moving. Rasagiline does not cure Parkinson's disease, but it does help to manage symptoms by increasing the amount of dopamine, a substance in the brain that helps control movement and mood.
Rasagiline Slowing Parkinson's Progression
The potential of Rasagiline to slow the progression of Parkinson’s disease has been a topic of much research. Studies have suggested that rasagiline may have neuroprotective properties that could help to delay the progression of this condition. These properties could help to preserve more of the brain’s dopamine-producing cells, which could in turn delay the worsening of symptoms.
Scientific Studies on Rasagiline
Several studies have been conducted to understand the impact of Rasagiline on Parkinson's disease. In one study, it was found that early and continuous treatment with rasagiline at a dose of 1 mg per day provided benefits that were consistent with a possible disease-modifying effect, such as a delayed start to levodopa treatment.
Side Effects of Rasagiline
Like all medications, Rasagiline has its side effects. Some of the most common side effects include joint pain, depression, indigestion, and weight loss. However, the benefits of this drug, in terms of managing symptoms and potentially slowing the progression of the disease, often outweigh these side effects. As always, it is important to discuss any concerns with your healthcare provider.
Interactions and Precautions with Rasagiline
There are certain drug interactions and precautions to be aware of when taking rasagiline. For instance, it can have interactions with antidepressants and other drugs for Parkinson's. Additionally, it should be used with caution in patients with a history of heart disease or hypertension. It is always important to inform your doctor about all the medications you are currently taking.
Treatment Plan with Rasagiline
It is important to remember that every person with Parkinson's disease is unique and will respond differently to treatment. Therefore, a treatment plan with rasagiline should be tailored to the individual’s specific symptoms and needs. Regular follow-ups with your healthcare provider are crucial to monitor the effectiveness of the medication and to make necessary adjustments.
Conclusion: The Future of Parkinson's Treatment with Rasagiline
While Parkinson's disease is a progressive condition, advancements in treatment, like rasagiline, offer hope to those diagnosed. Rasagiline has shown promise in controlling symptoms and potentially slowing disease progression. As research continues, it is hopeful that we will gain a deeper understanding of how this drug, and others like it, can provide an even greater benefit to those living with Parkinson's disease.

Anthony Palmowski
July 1, 2023 AT 16:45Rasagiline? More hype than help!!!
Jillian Rooney
July 17, 2023 AT 21:39Honestly, the U.S. has some of the best neurologists, but we keep pushing shiny pills like Rasagiline without real proof. It's a classic case of marketing over science, and it makes my blood boil. People think a cheap MAOI will magically stop neurodegeneration – nonsense! The side‑effects are real, and the hype distracts from lifestyle changes. We need to be honest with patients, not sell them hopes they can’t keep.
Rex Peterson
August 2, 2023 AT 12:39The discourse surrounding disease‑modifying agents such as rasagiline must be situated within a broader epistemological framework. While empirical trials suggest a modest delay in levodopa initiation, one must interrogate the causal mechanisms posited. Is the observed benefit a true neuroprotective effect, or merely a symptomatic amelioration that alters clinical endpoints? Moreover, the heterogeneity of Parkinsonian phenotypes complicates any universal assertion of efficacy. Ethical considerations also emerge when prescribing a medication with ambiguous long‑term outcomes. Nonetheless, the therapeutic landscape benefits from rigorous scrutiny. Continual meta‑analysis will elucidate whether rasagiline transcends adjunctive status. In sum, cautious optimism should guide clinical decision‑making.
Candace Jones
August 17, 2023 AT 13:45Rasagiline can certainly complement a broader treatment plan, especially when titrated carefully. Monitoring for depression and joint discomfort is advisable. Always coordinate adjustments with your neurologist to maintain balance.
Robert Ortega
September 1, 2023 AT 00:59From a neutral standpoint, the data on rasagiline's disease‑modifying potential remains mixed. Some patients report noticeable stability, while others see little change. It’s important to weigh personal experience against clinical evidence.
Elizabeth Nisbet
September 14, 2023 AT 22:19Exactly, staying attuned to individual response is key. Keep a symptom diary and bring it to appointments. That way you and your doctor can make informed tweaks.
Sydney Tammarine
September 28, 2023 AT 05:45Oh dear, another miracle cure in the pipeline! 🌟 Rasagiline is being thrust upon us like the latest fashion accessory, and everyone pretends it’s a panacea. The drama! The hype! The endless press releases that promise to halt the inexorable march of neurodegeneration. Yet, beneath the glitter lies the stark reality of side‑effects and modest benefits. 🙄 Let’s not forget that true progress comes from patience, research, and not from swallowing every shiny pill.
josue rosa
October 10, 2023 AT 23:19Indeed, the pharmacodynamic profile of rasagiline warrants a meticulous examination that extends beyond superficial efficacy claims. Firstly, rasagiline functions as an irreversible inhibitor of monoamine oxidase‑B, thereby augmenting synaptic dopamine concentrations, a mechanism which theoretically mitigates dopaminergic neuronal attrition. Secondly, preclinical investigations have illuminated its capacity to up‑regulate anti‑apoptotic pathways such as Bcl‑2, while concurrently attenuating oxidative stress markers like malondialdehyde, suggesting a potential neuroprotective axis. Thirdly, clinical data from the ADAGIO trial, albeit contentious, indicated that early initiation at 1 mg daily correlated with a delayed need for levodopa escalation, an outcome that may reflect disease‑modifying properties rather than mere symptomatic relief. Fourthly, the drug’s pharmacokinetics reveal a relatively stable plasma half‑life, facilitating once‑daily dosing and optimizing patient adherence, which is a non‑trivial factor in chronic disease management. Fifthly, the adverse effect spectrum, including but not limited to joint discomfort, depressive symptoms, and gastrointestinal disturbances, must be contextualized within a risk‑benefit paradigm, particularly for patients with comorbid cardiovascular conditions wherein MAO‑B inhibition could precipitate hypertensive crises if dietary tyramine restrictions are violated. Sixthly, drug‑drug interactions, especially with serotonergic agents, merit vigilant monitoring due to the heightened risk of serotonin syndrome. Seventhly, biomarker analyses employing neuroimaging modalities such as DaT‑SPECT have yielded equivocal findings regarding dopaminergic terminal preservation, underscoring the necessity for longitudinal studies with robust endpoints. Eighthly, the heterogeneity of Parkinsonian subtypes-tremor‑dominant versus akinetic‑rigid phenotypes-may modulate therapeutic responsiveness, thereby advocating for a personalized medicine approach. Ninthly, health economics considerations cannot be ignored; cost‑effectiveness analyses suggest that rasagiline’s incremental cost may be offset by reduced levodopa‑associated dyskinesias and healthcare utilization. Tenthly, patient‑reported outcome measures (PROMs) have demonstrated modest improvements in quality‑of‑life indices, yet the clinical significance remains debated. Eleventhly, the ethical discourse surrounding early pharmacologic intervention in a disease with variable progression trajectories raises questions about overtreatment. Twelfthly, ongoing trials investigating combination therapies with neurotrophic factors may elucidate synergistic effects. Thirteenthly, regulatory perspectives differ globally, influencing accessibility and prescribing patterns. Fourteenthly, real‑world evidence from registries continues to augment our understanding of long‑term safety. Fifteenthly, the integration of rasagiline into multimodal treatment algorithms should be predicated on a comprehensive assessment of disease stage, patient preferences, and comorbidities. Finally, while the promise of disease modification remains enticing, the scientific community must persist in rigorous, controlled investigations to substantiate these claims beyond anecdotal optimism.
Shawn Simms
October 23, 2023 AT 02:59The discussion above reflects a balanced appraisal of rasagiline’s therapeutic profile. It is essential to distinguish between statistically significant findings and clinically meaningful outcomes. Moreover, adherence to guideline‑based prescribing ensures patient safety. Continued surveillance for adverse events remains paramount. Ultimately, informed consent should encompass both potential benefits and limitations.