Understanding Chronic Diarrhea and Its Causes
As someone who has experienced chronic diarrhea, I know how frustrating and debilitating it can be. Chronic diarrhea refers to the frequent passing of loose or watery stools, lasting for more than four weeks. There are various causes of chronic diarrhea, such as infections, food intolerances, and certain medications. However, one of the most significant causes of chronic diarrhea is inflammatory bowel disease (IBD).
IBD is an umbrella term used to describe a group of disorders that cause chronic inflammation in the digestive tract. The two most common forms of IBD are Crohn's disease and ulcerative colitis. Both conditions can lead to chronic diarrhea and severely impact a person's quality of life. In this article, we will explore the connection between chronic diarrhea and IBD to better understand these conditions and how to manage them.
Recognizing the Symptoms of Inflammatory Bowel Disease
Before we dive into the connection between chronic diarrhea and IBD, it's essential to understand the symptoms that may indicate the presence of an inflammatory bowel disease. In addition to chronic diarrhea, people with IBD may experience abdominal pain, cramping, fatigue, weight loss, and blood in the stool. These symptoms can vary in severity and duration, making it challenging to pinpoint an IBD diagnosis.
If you or someone you know is experiencing these symptoms, it's crucial to consult with a healthcare professional to determine whether IBD could be the underlying cause. Early diagnosis and treatment can significantly improve the management of IBD and help alleviate chronic diarrhea and other debilitating symptoms.
How Inflammatory Bowel Disease Causes Chronic Diarrhea
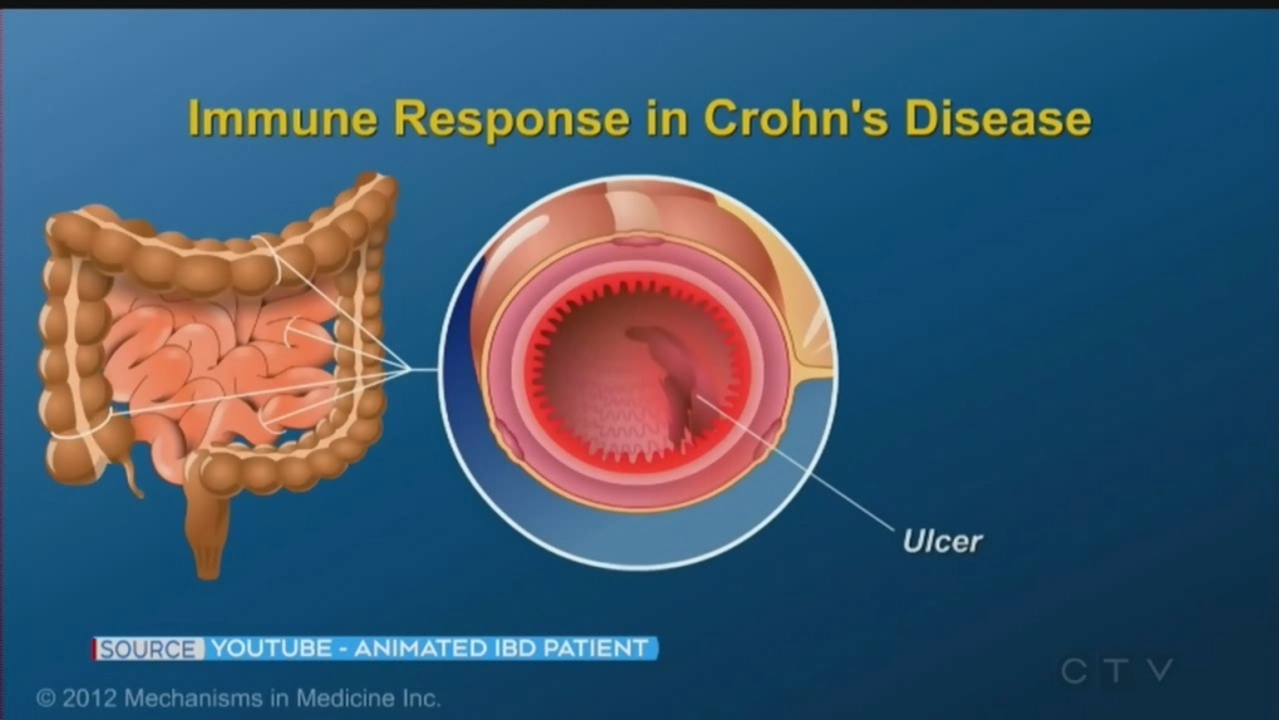
Now that we've established the symptoms of IBD let's explore how these conditions can lead to chronic diarrhea. Inflammatory bowel diseases, such as Crohn's disease and ulcerative colitis, cause inflammation in the digestive tract. This inflammation can disrupt the normal functioning of the intestines, leading to the increased movement of food and water through the digestive system.
As a result, the body doesn't have enough time to absorb water from the stool, leading to loose and watery stools. This process is what causes diarrhea in individuals with IBD. Additionally, the inflammation can also damage the lining of the intestines, making it harder for the body to absorb nutrients and maintain proper bowel function.
Managing Chronic Diarrhea in IBD Patients
Living with chronic diarrhea and IBD can be challenging, but there are ways to manage these conditions and improve your quality of life. One of the most important aspects of managing IBD and chronic diarrhea is working with a healthcare professional to develop a personalized treatment plan. This plan may include medications to reduce inflammation, dietary modifications, and other lifestyle changes.
For example, some people with IBD find that avoiding certain foods, such as spicy foods, high-fat foods, or foods high in fiber, helps alleviate their chronic diarrhea. Additionally, staying hydrated and consuming smaller, more frequent meals can also aid in managing diarrhea and other IBD symptoms.
Seeking Support and Coping with the Emotional Impact of IBD
Dealing with chronic diarrhea and IBD can take an emotional toll on individuals and their loved ones. It's crucial to seek support from friends, family, and healthcare professionals to help cope with the emotional aspects of living with a chronic illness. Joining a support group for people with IBD can also be beneficial, as it provides an opportunity to connect with others who understand the challenges of living with these conditions.
Moreover, practicing stress management techniques, such as deep breathing exercises, meditation, and engaging in hobbies or activities you enjoy, can help improve your overall well-being and make it easier to cope with the daily struggles of living with IBD and chronic diarrhea.
Final Thoughts on Chronic Diarrhea and Inflammatory Bowel Disease
Understanding the connection between chronic diarrhea and inflammatory bowel disease is crucial for those living with these conditions. By recognizing the symptoms of IBD and seeking appropriate medical care, individuals can improve their quality of life and manage chronic diarrhea more effectively.
It's essential to work with healthcare professionals to develop a personalized treatment plan and seek support from friends, family, and support groups. Managing IBD and chronic diarrhea is possible, and with the right resources and support, you can live a fulfilling life despite these challenges.

steve wowiling
May 19, 2023 AT 20:23Ever wonder why our guts seem to have a mind of their own, like a rebellious philosopher trapped in a wet tube?
Chronic diarrhea feels like the universe is shouting, “Pay attention!” while the colon just shrugs.
Inflammation in IBD is the drama queen of the digestive tract, turning every meal into a performance.
When the lining gets angry, it forgets its job of absorbing water, and we’re left with a never‑ending stream.
It’s almost poetic, the way our bodies betray us when they’re under siege.
But the good news? Modern therapies can calm down that diva and give us back some dignity.
Warren Workman
May 25, 2023 AT 09:33From a pathophysiological standpoint, the mucosal immune dysregulation supersedes simplistic “water‑loss” narratives.
One must consider the cytokine cascade-TNF‑α, IL‑12/23-and their impact on epithelial tight junction integrity.
Therefore, attributing chronic diarrhea solely to “inflammation” lacks granularity.
Clinical management should prioritize molecular targeting over anecdotal symptom suppression.
Kate Babasa
June 5, 2023 AT 23:20I totally get that dealing with IBS‑like symptoms can feel isolating, and it’s important to remember we’re not alone in this.
There’s a growing body of evidence that suggests diet, stress management, and even gut microbiota modulation play pivotal roles.
Moreover, interdisciplinary care-gastroenterology, nutrition, psychology-offers a more holistic approach.
Don’t underestimate the power of supportive communities, whether online or in‑person, to share coping strategies!
In short, while medication is essential, lifestyle tweaks can synergistically improve outcomes.
king singh
June 17, 2023 AT 13:06Totally agree, small changes add up over time.
Adam Martin
June 29, 2023 AT 02:53Look, the whole “chronic diarrhea equals just a bad day” narrative is a gross oversimplification that does a disservice to anyone battling IBD.
First, the intestinal mucosa isn’t merely a passive barrier; it’s an active immune organ constantly sampling antigens, and when that system goes haywire, the result is a cascade of cytokines, chemokines, and cellular infiltrates that wreak havoc on water absorption.
Second, the dysbiosis observed in many Crohn’s and ulcerative colitis patients alters short‑chain fatty acid production, further compromising electrolyte balance and stool consistency.
Third, the neuro‑enteric axis means that stress hormones like cortisol can exacerbate motility issues, turning a calm gut into a hyperactive torrent.
Fourth, let’s not forget that many mainstream treatments-steroids, immunomodulators-have side effects that themselves can precipitate diarrheal episodes.
Fifth, dietary triggers such as FODMAPs or specific fibers can vary wildly between individuals, making a one‑size‑fits‑all diet plan meaningless.
Sixth, the chronic inflammatory state leads to microscopic ulcerations, which bleed subtly and further irritate the bowel wall.
Seventh, the body’s compensatory mechanisms, like increased secretory chloride channels, can unintentionally amplify fluid loss.
Eighth, the psychological burden-anxiety, depression-can feed back into gut dysmotility, creating a vicious cycle that’s hard to break.
Ninth, research shows that early biologic intervention can modulate the disease trajectory, reducing the frequency of watery stools in many patients.
Tenth, patient education about hydration, electrolyte replacement, and safe medication use is crucial for preventing secondary complications.
Eleventh, support groups provide emotional scaffolding that can improve adherence to complex treatment regimens.
Twelfth, regular monitoring with colonoscopy or non‑invasive biomarkers helps tailor therapy before irreversible damage occurs.
Thirteenth, telemedicine platforms now allow for rapid symptom reporting, enabling timely adjustments.
Fourteenth, integrating mindfulness or yoga can lower stress‑induced flares, though evidence is still emerging.
Fifteenth, ultimately, managing chronic diarrhea in IBD is a multidimensional challenge that demands a personalized, evidence‑based strategy rather than a blanket “just drink water” slogan.
Ryan Torres
July 10, 2023 AT 16:40🤔🤬 The pharma giants don't want you to know that most of these “advanced biologics” are just a cash‑grab, and the real cause is the hidden surveillance of our gut microbiome by secret societies! 🌐💊 Stay woke, hydrate, and question every prescription they push on you. 😤🚨
shashi Shekhar
July 22, 2023 AT 06:26Honestly, all this talk about cytokines and microbiomes feels a bit overblown for most folks just trying to get through the day without running to the bathroom every five minutes.
If you stick to basic stuff-avoid spicy curry, drink enough water, maybe try a probiotic-you’ll see decent relief without diving into a PhD‑level lecture.
Also, don’t get sucked into every new “miracle” supplement that promises a cure; most of them are just marketing fluff.
Marcia Bailey
August 14, 2023 AT 10:00Hey, I totally hear you! 🌟 It’s easy to feel overwhelmed, but remember that small, consistent steps-like a balanced diet, gentle exercise, and keeping a symptom diary-can make a huge difference.
Don’t hesitate to lean on your healthcare team; they’re there to help fine‑tune your plan.
And if you ever need a listening ear or more tips, I’m here! 😊