Picture this: You wake up in a hospital bed after a heart scare. Nurses check your pulse. Your doctor walks in, calm but serious, and starts talking about a new pill you're supposed to take every single day. It's called Plavix. Sounds intimidating, right? Suddenly, your life depends on a small tablet and a lot of information you never expected to need. But what does Plavix really do, why is it so important, and is it actually as scary as it sounds?
What Exactly Is Plavix and How Does It Work?
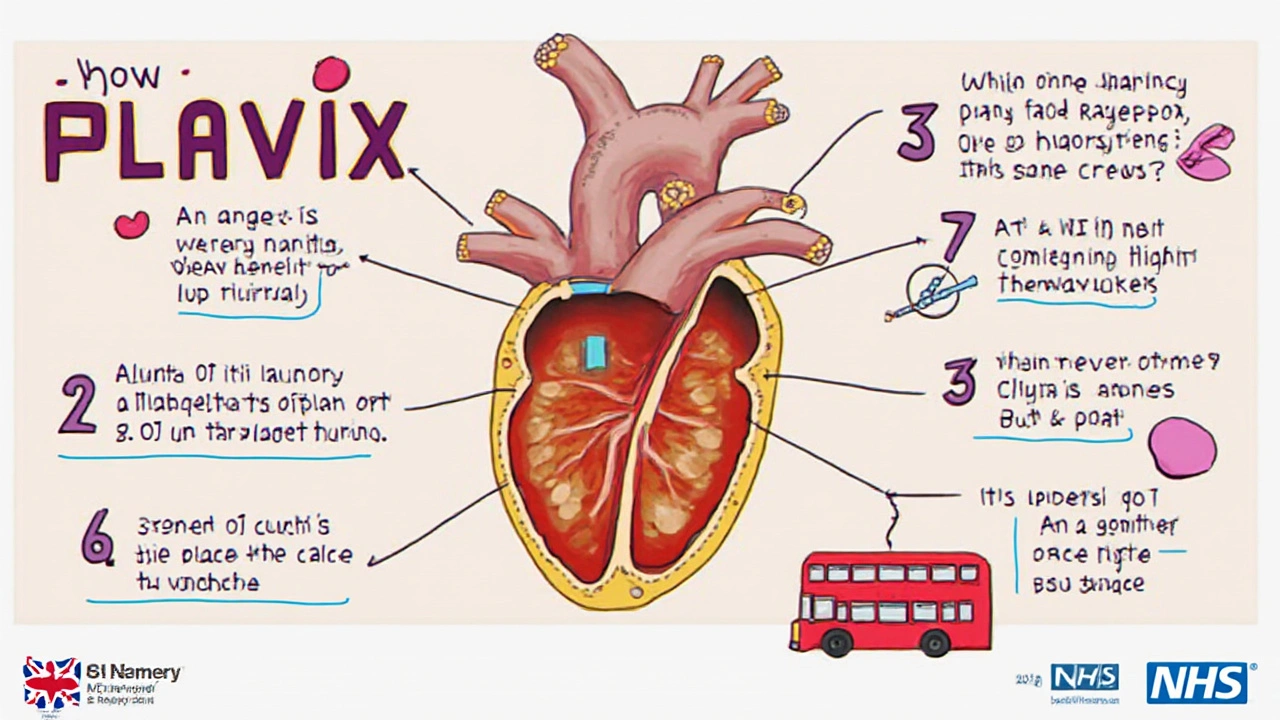
If someone you know has ever experienced a heart attack or stroke, there's a pretty high chance they've heard the name Plavix tossed around. But here's the thing: Plavix (known by its generic name clopidogrel) isn’t just another heart medicine. It’s a kind of blood thinner, but not in the way blood thinners like warfarin work. Instead, Plavix is an antiplatelet, meaning it keeps your platelets—those tiny cell fragments in your blood—from clumping together and forming dangerous clots. Think of it like Teflon for your blood vessels: it makes it harder for platelets to stick together at the wrong time, which helps reduce your risk of a new heart attack or a stroke caused by a clot.
The science behind it gets wild. Platelets rush to any spot where your skin breaks, or where a blood vessel is damaged, and they clog it up to stop bleeding. Normally, that's great! But if you have blocked arteries, even a minor irritation inside your blood vessel can set off an unnecessary clot, and a clot in the wrong place can block blood flow to your heart or brain. According to the FDA, Plavix has been a cornerstone in treating acute coronary syndrome and for patients with stents in their arteries for more than two decades. After its approval in 1997, it changed how doctors approach heart attack prevention forever.
A fun fact: Over 40 million prescriptions for Plavix have been filled in the U.S. just in the last decade. That's a lot of people trusting this tiny pill to keep their blood flowing smoothly. The most common dosage is 75 mg once a day, but in some situations, a higher loading dose gets things started faster after certain procedures.
This all sounds pretty technical, but trust me—your body notices the difference. With fewer sticky platelets roaming your arteries, you seriously cut down on the risk of a life-threatening clot. The Antithrombotic Trialists' Collaboration reviewed studies with hundreds of thousands of patients and found a clear pattern: antiplatelet therapy, especially clopidogrel, lowers the odds of recurrent heart attacks and strokes. That’s not small potatoes. And, according to the American Heart Association, it remains one of their top recommendations after a big heart event.
Who Should—and Shouldn’t—Use Plavix?
Doctors love Plavix for people with a high risk of clotting. This usually means anyone who’s had a recent heart attack, an ischemic stroke, or a procedure like angioplasty to open up narrow arteries, especially if a stent (a tiny mesh tube) was placed. You might also get on Plavix after a type of chest pain called unstable angina—basically, chest pain that means your heart is starved for oxygen because of blockages in the arteries.
There’s also a group that benefits from Plavix but doesn’t always realize it. Folks with peripheral artery disease (PAD)—where arteries in your legs are blocked—may be prescribed Plavix to keep things moving and ward off serious complications. If your doctor once said something about blood flow in your extremities, you were probably in this group.
But here’s where it gets tricky: not everyone is a great match for Plavix. If you have bleeding disorders, recent internal bleeding, or severe liver disease, this medication can do more harm than good. Pregnant or breastfeeding? Plavix isn’t usually the go-to. And if you’re taking certain other meds—think proton pump inhibitors like omeprazole for acid reflux, or other blood thinners like warfarin—those combinations may weaken or boost the effects in ways you don’t want.
Genetic differences also play a surprising—and honestly, a bit annoying—role. Some people have liver enzymes that don’t activate Plavix well, so it doesn’t work as expected. A genetic test can show if you’re in that group (especially common in people of Asian descent). If your body can’t turn the drug into its active form, you might need an alternative like ticagrelor or prasugrel. But don’t stress about memorizing these names—your cardiologist will know the drill.
Timing is another big deal. Plavix isn’t something you just pop as needed. Stopping it too soon after a stent, for example, can put you in real danger for a clot. There’s tons of evidence for that: a study in the New England Journal of Medicine found that people who stopped Plavix early after stent placement were at much greater risk for major heart problems. If your doctor says “keep taking it until we say stop,” that’s the real deal—not just a suggestion.
Surprising Facts, Myths, and Tips About Plavix
First, let’s blow up a few myths. No, Plavix doesn’t turn your blood into water. People sometimes think they’ll bleed out from the tiniest scratch—but while Plavix does raise the chance of bruising or nosebleeds, dramatic bleeding is actually rare unless you’re also on other blood thinners or have underlying issues. A scraped knee in the backyard isn’t going to be a medical emergency now. But you will want to watch for unusual bleeding—like blood in your urine or stools, dark tarry stools, or unexplained large bruises. Head injuries need special caution, since even a minor bump could cause a dangerous bleed. If you ever hit your head while on Plavix, don’t wait—get checked.
Eating and drinking on Plavix gets a lot of questions. Can you still have the occasional glass of wine? Most doctors say a little alcohol is fine, but heavy drinking raises the risk of stomach bleeds. About diet: there’s no special food list to follow, but coupling Plavix with leafy greens or vitamin K isn’t a problem (not like with warfarin, where those foods can mess up your dose).
If you need surgery or even dental work, it’s important your medical providers know you’re on Plavix. Sometimes, your doctor may tell you to stop Plavix a few days before surgery to lower bleeding risk, but never just decide to skip it on your own. One UK surgeon famously said, “It’s easier to fix bleeding than to fix a clot that’s killed part of the heart or brain.” Good to remember.
Here’s a strange but true tip: some people notice their urine smells sweet or odd while on Plavix. If you spot changes like that, raise it with your doctor—but don’t panic. It’s usually harmless. Another interesting nugget: Plavix comes with a “black box” warning in the U.S. for the genetic enzyme issue mentioned above, so if your doctor suggests a test before starting, it’s not overkill—it’s real medicine catching up with real life.
Refilling your prescription on time is one of the smartest moves you can make. Missing doses for a few days, especially in the first year after a stent or heart attack, is like driving without airbags. Mark your calendar, use pill boxes—whatever works so you don’t miss a beat.
And no, there’s nothing magic about brand name versus generic. As of 2012, clopidogrel is available as a generic and works just as well as the brand-name Plavix (you’ll save a ton at the pharmacy).
What Side Effects Should You Watch For and When Should You Call the Doctor?
No pill is perfect, and Plavix is no exception. The most common side effects are bruising and minor bleeding—nosebleeds, gum bleeding, or easy bruising are just part of the deal for some folks. Less often, you might get diarrhea, rashes, or itchy skin. Most of these are annoying rather than dangerous, but anything new after starting Plavix is worth mentioning to your healthcare provider.
Here’s what’s more serious: big or unexpected bleeding. Blood in your stool (which can look black and tarry), urine, or vomiting something that looks like coffee grounds needs quick attention. If you find yourself feeling weak, super pale, or short of breath, those could be signs you’re losing blood inside. Rarely, Plavix can trigger a severe allergic reaction—trouble breathing, swelling of your face or tongue, or a spreading rash. Head to the ER if you ever notice those.
A wild but true fact: Plavix can—very rarely—trigger a dangerous condition called thrombotic thrombocytopenic purpura (TTP). The Mayo Clinic describes it as a sudden drop in platelets, with symptoms like purple spots on your skin and fever. It’s rare enough that most cardiologists have never even seen a case, but if you notice purple dots, confusion, or unexplained fever while on Plavix, don’t wait. As Dr. Deepak Bhatt at Harvard Medical School says:
“While Plavix offers lifesaving benefits after a heart event, patients and doctors need to watch for both minor and more serious bleeding signs—cautious teamwork is key.”
Keep a list of any symptoms that seem odd or new since starting the medication. Bring the list to your check-ups. If you’re ever unsure, pharmacists are a great resource—they understand this stuff inside and out.
One more thing: older adults are a bit more sensitive to Plavix’s effects, especially if they’re on lots of other meds. Always double-check before adding any over-the-counter or herbal products—some, like NSAIDs (ibuprofen), increase bleeding risk if you mix them in. When in doubt, call and ask. Better safe than sorry.
And the biggest tip? Don’t be shy about asking your doctor questions. Plavix is a serious med, but it can change—maybe even save—your life. If something feels off, trust your gut and get it checked. There’s a reason it’s become one of the most-prescribed heart drugs in history—it works, but only if you use it smartly.


Deborah Escobedo
June 14, 2025 AT 12:32Plavix can feel intimidating but it’s really just a safeguard for your heart. Stay consistent with your doses and you’ll give yourself the best chance at a smoother recovery.
Dipankar Kumar Mitra
June 15, 2025 AT 09:22Ever wonder why a tiny tablet holds the power to keep a whole life from slipping away? It’s like the universe whispering, “don’t rush the river,” while your blood silently obeys. You’re not just taking a drug; you’re honoring the fragile dance between clot and flow. Keep it steady, and let the science do its quiet work.
Tracy Daniels
June 16, 2025 AT 06:12For anyone starting Plavix, it’s essential to track any unusual bruising or nosebleeds 😊. Consistency is key-set a daily reminder and keep a small pill organizer. If you experience any gastrointestinal discomfort, discuss it with your pharmacist; they can suggest taking it with food to lessen irritation.
Hoyt Dawes
June 17, 2025 AT 03:02Oh please, another “life‑changing” pill? We’re all fed the same hype while pharma pockets the profits. If you actually want to feel alive, stop obsessing over brand names and just swallow what the doctor wrote. Drama aside, the pill does its job-no miracles here.
Jeff Ceo
June 17, 2025 AT 23:52Listen up-don’t skip doses because you think you’re “fine”. Missing even a single day after a stent can invite a clot that could undo months of recovery. Take the medication as prescribed, period.
David Bui
June 18, 2025 AT 20:42Right, let’s cut the fluff. Plavix works by blocking the P2Y12 receptor on platelets, which means those little blood‑clot machines can’t stick together like they usually do after an injury. That’s why it’s a go‑to after PCI or for anyone with a history of MI. But watch out for drug interactions-omeprazole can blunt its activation, so your doc might switch you to pantoprazole instead. Also, if you’re on NSAIDs, you’re upping your bleed risk-keep that in mind when you pop ibuprofen for a headache. Bottom line: it’s effective when you follow the protocol.
Alex V
June 19, 2025 AT 17:32Sure, “the pill saves lives,” they say, while the big pharma lobbyists grin behind the curtain. Ever notice how every new “miracle” comes with a black‑box warning that no one really reads? If you’re skeptical, read the FDA briefing yourself instead of swallowing the PR fluff. Your blood doesn’t need a chemical leash unless you let the system tell you otherwise.
Robert Jackson
June 20, 2025 AT 14:22Honestly, the UK NHS got this sorted ages ago-just follow the script and don’t overthink it.
Maricia Harris
June 21, 2025 AT 11:12Another pill to add to the mountain of meds? Just what I needed, said no one ever.
Tara Timlin
June 22, 2025 AT 08:02Hey folks, if you’re wondering about alcohol with Plavix, a couple of glasses of wine won’t mess things up, but binge drinking can increase bleeding risk. Also, make sure to inform any dentist before procedures-they might ask you to pause the pill for a few days. Stay on top of refill dates; a missed dose can feel like a tiny time bomb waiting to go off.
Jean-Sébastien Dufresne
June 23, 2025 AT 04:52Deborah, you’re right-consistency is the unsung hero here! 🎯 The real challenge is remembering to take it every day, especially when life gets chaotic. A simple phone alarm or a sticky note on the fridge can make all the difference; trust me, you’ll thank yourself later.
Patrick Nguyen
June 24, 2025 AT 01:42Dipankar, you’ve captured the philosophical angle nicely. In plain terms, the drug’s antiplatelet action reduces thrombotic events, which aligns with your metaphor of the river.
Patrick Bread
June 24, 2025 AT 22:32Tracy, the reminder tip is gold. Also, if you ever notice black stools, that’s a red flag-don’t wait, seek help immediately.
Fiona Doherty
June 25, 2025 AT 19:22Hoyt, I get the frustration, but dismissing proven therapy does more harm than good. The drug isn’t a cash grab; it’s evidence‑based and has saved countless lives.
Neil Greer
June 26, 2025 AT 16:12Jeff, spot on about the importance of adherence. Missing doses isn’t just a slip-it’s a real risk for re‑occlusion.
Fionnuala O'Connor
June 27, 2025 AT 13:02David, clear explanation-thanks. Keep an eye on those drug interactions and you’ll stay safe.
Christopher MORRISSEY
June 28, 2025 AT 09:52The concerns you raise about pharmaceutical influence merit a measured discussion rather than outright dismissal.
While it is true that commercial interests can shape the narrative surrounding medications, the clinical data on clopidogrel are robust and have been replicated across numerous trials.
Large‑scale studies such as CURE and TRITON have demonstrated a clear reduction in composite cardiovascular endpoints when patients adhere to antiplatelet therapy.
Moreover, the regulatory review process employed by agencies like the FDA and EMA involves rigorous scrutiny of efficacy and safety profiles.
It is therefore inaccurate to suggest that the drug’s benefits are merely a product of marketing hype.
Patients who have experienced myocardial infarction or received stents are routinely placed on Plavix because the evidence supports its role in preventing stent thrombosis, a dreaded complication.
That said, vigilance is essential; clinicians must remain aware of the drug’s interaction potential and the rare but serious adverse events you mentioned.
Pharmacogenomic testing, for instance, can identify individuals with reduced CYP2C19 activity who may derive less benefit from clopidogrel.
In such cases, an alternative antiplatelet agent like ticagrelor might be more appropriate, illustrating how personalized medicine can mitigate the very concerns you raise.
The black‑box warning you referenced is not a scare tactic but a transparent acknowledgment of a specific risk factor.
When patients and providers engage in open dialogue about these risks, adherence improves and outcomes are optimized.
It is also worth noting that the cost of generic clopidogrel has decreased substantially, making it accessible to a broader population.
This economic aspect further counters the notion that the drug exists solely to enrich manufacturers.
Ultimately, a balanced perspective that weighs both the drug’s proven efficacy and its limitations fosters better patient empowerment.
I encourage readers to consult their healthcare providers, review the latest guidelines, and, if needed, seek a second opinion to address any lingering doubts.
By doing so, we move beyond conspiratorial rhetoric and embrace evidence‑based stewardship of cardiovascular health.