Meclizine Drug Interaction Checker
Check Your Medication Safety
Meclizine interacts with many common medications. This tool helps identify potential dangerous combinations based on the article content. Always consult your doctor before making changes to your medications.
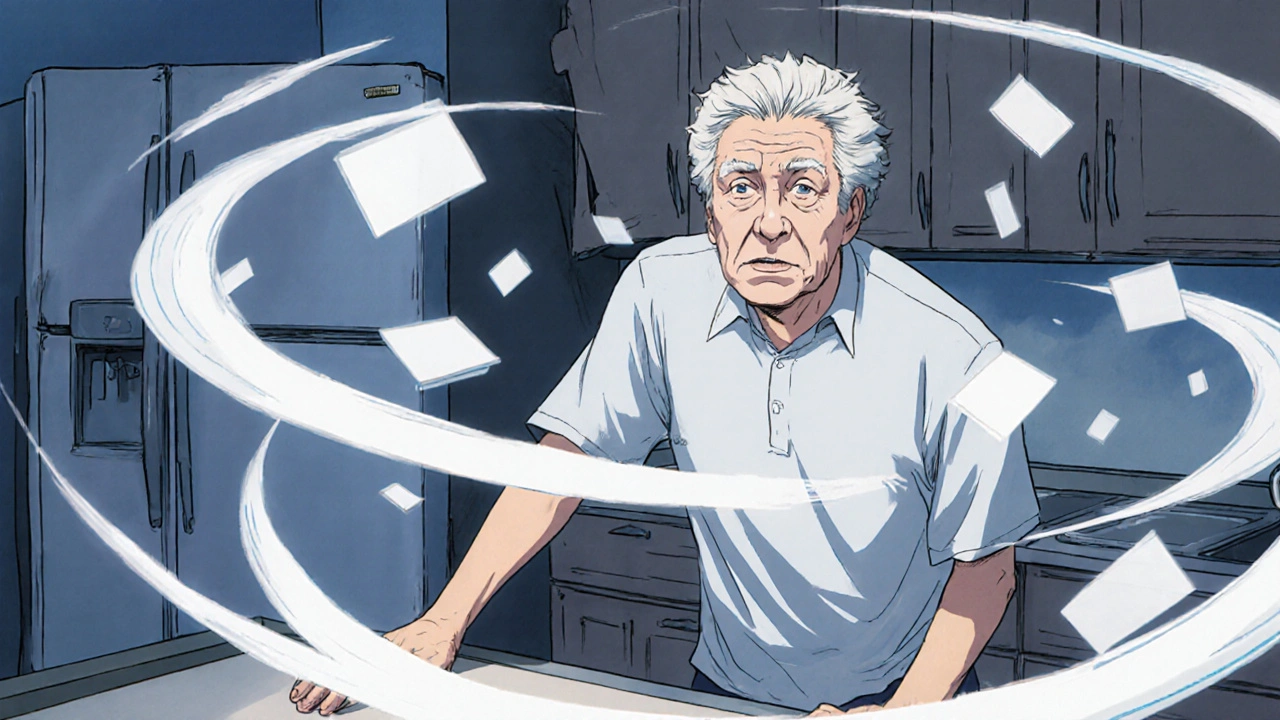
When vertigo hits, it doesn’t just make you feel dizzy-it can turn a simple walk to the kitchen into a dangerous tumble. For many people, meclizine is the first medication their doctor reaches for. It’s been around since the 1970s, sold under names like Antivert and Dramamine Less Drowsy, and still widely prescribed today. But knowing it works isn’t the same as knowing how it affects your body, especially if you’re taking it regularly or mixing it with other meds.
How Meclizine Stops Vertigo
Meclizine doesn’t fix the root cause of vertigo-whether it’s from an inner ear infection, BPPV, or even a migraine. Instead, it quietly calms the confusion in your brainstem. It blocks histamine receptors in the vestibular system, the part of your inner ear that tells your brain which way is up. But here’s the twist: it also has strong anticholinergic effects, meaning it messes with acetylcholine, a brain chemical tied to balance, memory, and alertness.
This dual action is why meclizine works so well for sudden dizziness. Studies from 1972 showed it reduced vertigo symptoms by an average of 40% on a 100-point scale-far better than a sugar pill. More recent research from 2020 found it doesn’t shut down your vision or inner ear signals like older drugs did. Instead, it helps your brain adapt faster to the mismatch between what your eyes see and what your inner ear feels. That’s why doctors say it helps your body “maintain its sense of balance.”
Common Side Effects: It’s Not Just Drowsiness
Most people know meclizine makes you sleepy. But that’s just the tip of the iceberg. In fact, drowsiness is so common that the Mayo Clinic explicitly warns: “Do not drive or operate machinery until you know how this medicine affects you.” That’s not a suggestion-it’s a safety rule backed by real-world reports of people crashing their cars because they took the pill at breakfast and felt foggy by noon.
Other frequent side effects include:
- Dry mouth
- Blurred vision
- Constipation
- Difficulty urinating
- Headache
- Feeling unusually tired or weak
These aren’t rare. Up to 30% of users report at least one of these symptoms. Dry mouth and blurred vision? Classic anticholinergic effects. They happen because meclizine blocks the same receptors that control saliva and pupil dilation. If you’re already on medication for high blood pressure, depression, or allergies, these side effects can pile up. That’s why doctors tell you to check with them before mixing meclizine with cold medicines, sleep aids, or even over-the-counter antihistamines like diphenhydramine.
Who Should Avoid Meclizine
Meclizine isn’t safe for everyone. If you’re over 65, you’re at higher risk for serious side effects. Older adults are more sensitive to anticholinergic drugs, and even a 25 mg dose can lead to confusion, falls, or urinary retention. The American Geriatrics Society lists meclizine as a potentially inappropriate medication for seniors because of this.
People with glaucoma should avoid it-it can raise eye pressure. Those with enlarged prostate or bladder problems may find it harder to pee. Pregnant women should talk to their doctor before using it, though it’s sometimes used for morning sickness when other options fail. And if you’ve ever had an allergic reaction to meclizine or similar drugs like dimenhydrinate, skip it entirely.
One big myth: meclizine is safe for long-term use. It’s not. While it’s great for short flare-ups-say, during a bout of vestibular neuritis-it’s not meant for daily, month-long use. The longer you take it, the more your brain gets used to the chemical fog. That can delay natural recovery. Vestibular rehabilitation exercises, physical therapy, and balance training often work better over time and don’t come with a foggy brain.

Dosing: When and How to Take It
Dosing is simple, but timing matters. For vertigo, most people take 25 mg once a day. For motion sickness, take it 1 hour before travel. Some brands offer 12.5 mg tablets for milder cases or for older adults. Chewable tablets are available if swallowing pills is hard.
Take it with water. Don’t crush or split tablets unless your doctor says so. Don’t double up if you miss a dose-just skip it and go back to your regular schedule. And never take it with alcohol. Even one drink can turn mild drowsiness into dangerous sedation.
Most people feel relief within 30 to 60 minutes. Effects last about 8 to 24 hours, depending on your metabolism. If you’re still dizzy after 3 days, or if symptoms get worse, call your doctor. That could mean your vertigo isn’t caused by something meclizine can help.
Drug Interactions: The Hidden Danger
Meclizine doesn’t play well with others. It’s a CNS depressant, meaning it slows down your brain. Combine it with:
- Alcohol
- Benzodiazepines (like diazepam or lorazepam)
- Opioid painkillers
- Antidepressants (especially tricyclics like amitriptyline)
- Sleeping pills (like zolpidem)
- Other antihistamines (even Benadryl)
Each of these can multiply the sedative effect. One study found that people taking meclizine with a sleep aid were 3 times more likely to fall. That’s not a small risk-it’s a hospital visit waiting to happen.
Even OTC cold medicines can be dangerous. Many contain diphenhydramine or doxylamine-both antihistamines. If you’re already on meclizine, adding a nighttime cold tablet is like pouring gasoline on a fire. Your drowsiness skyrockets. Your risk of confusion and falls goes up. Always check labels. If it says “helps you sleep” or “for allergies,” think twice.

Meclizine vs. Other Vertigo Treatments
Is meclizine the best option? It depends. For quick relief during a vertigo attack, yes. But for long-term management, other options exist.
Betahistine is used in Europe and Australia for Ménière’s disease. It works differently-by improving blood flow in the inner ear. It’s less sedating but not as widely available in the U.S.
Dimenhydrinate (Dramamine) is stronger for motion sickness but causes more nausea and drowsiness than meclizine.
Benzodiazepines like clonazepam can help with severe vertigo, but they’re addictive and not meant for daily use.
None of these are perfect. Meclizine’s edge? It’s cheap, widely available, and works fast. But it’s not the only tool. Physical therapy, like the Epley maneuver for BPPV, often cures the problem without pills at all.
When to Call Your Doctor
Most side effects fade as your body adjusts. But if you notice any of these, get help right away:
- Severe dizziness or fainting
- Difficulty breathing or swallowing
- Rapid heartbeat or chest pain
- Severe confusion or memory loss
- Inability to urinate
- Yellowing of skin or eyes (sign of liver issues)
These are rare, but they’re serious. Also, if your vertigo doesn’t improve after 3 to 5 days, or if you start having new symptoms like hearing loss, ringing in the ears, or numbness on one side of your body, don’t wait. It could be something more than an inner ear issue.
Final Thoughts: Use Wisely
Meclizine is a reliable tool for acute vertigo. It’s been used for over 50 years, and it still works. But it’s not a cure. It’s a temporary shield against dizziness. And like any shield, it has weight. It slows you down. It clouds your thinking. It can make everyday tasks risky.
Use it only when needed. Don’t take it daily unless your doctor says so. Avoid mixing it with other sedatives. Watch for side effects in older adults. And always pair it with physical therapy if possible. The goal isn’t to numb your dizziness forever-it’s to help your brain relearn balance so you don’t need the pill at all.
Can meclizine cause long-term damage?
No, meclizine doesn’t cause permanent damage when used as directed. But long-term use can delay natural recovery from vertigo and increase the risk of side effects like confusion, falls, and urinary problems-especially in older adults. It’s meant for short-term relief, not daily maintenance.
Is meclizine addictive?
Meclizine is not addictive in the way opioids or benzodiazepines are. You won’t develop cravings or withdrawal symptoms. But your body can get used to it, making you feel more dizzy when you stop. That’s not addiction-it’s rebound vertigo. Tapering off slowly under medical supervision helps avoid this.
Can I take meclizine with high blood pressure medication?
Yes, but with caution. Meclizine doesn’t directly raise or lower blood pressure, but it can make you feel lightheaded, especially when standing up. If you’re on blood pressure meds, this dizziness can be worse. Talk to your doctor about timing doses and monitoring your blood pressure when you start meclizine.
Does meclizine help with nausea from food poisoning?
It can help, but it’s not the best choice. Meclizine works best for vertigo-related nausea, not stomach upset. For nausea from food poisoning or stomach bugs, ondansetron or domperidone are more targeted and don’t cause drowsiness. Meclizine might mask symptoms without treating the cause.
Is there a non-drowsy alternative to meclizine?
For vertigo, yes-vestibular rehabilitation therapy. For motion sickness, ginger supplements or acupressure wristbands have some evidence. In some countries, betahistine is used as a non-sedating alternative. But in the U.S., there’s no direct non-drowsy replacement. Newer drugs are still in trials. For now, meclizine’s drowsiness is the trade-off for its effectiveness.
Can children take meclizine?
Meclizine is not approved for children under 12 for vertigo. For motion sickness, some doctors may prescribe it off-label for older children, but only at lower doses and with close monitoring. Always consult a pediatrician-children are more sensitive to anticholinergic side effects like dry mouth, constipation, and confusion.

robert cardy solano
November 20, 2025 AT 09:25Been taking meclizine for my BPPV for like 6 months now. Honestly? It’s the only thing that keeps me from barfing when I roll over in bed. But yeah, the dry mouth is brutal. I keep a water bottle taped to my nightstand. Also, forgot to mention-I tried to drive to the store once after taking it and ended up parked outside a gas station for 20 minutes trying to remember where I was going. 😅
Brianna Groleau
November 21, 2025 AT 10:17Y’all are acting like meclizine is some kind of evil potion. I get it-it makes you sleepy. But have you tried vestibular rehab? I did 8 weeks of balance exercises with a PT and now I don’t even need the pill anymore. My grandma took it for years and ended up in the ER after a fall. It’s not the drug’s fault-it’s the mindset. We treat symptoms like they’re the enemy instead of signals. My therapist said, ‘Your brain forgot how to listen to your inner ear.’ Meclizine just turns down the volume. But rehab? That’s the teacher. And teachers don’t give you A’s for cheating.
Sarah Swiatek
November 21, 2025 AT 17:02Oh sweet mercy. Another person telling me to ‘just do physical therapy.’ Like that’s some magic cure-all for people who can’t even stand up without holding onto furniture. I’ve been doing Epley maneuvers for six months. Twice a day. My neck screams. My balance is still garbage. And now you want me to stop the one thing that lets me walk to the fridge without feeling like I’m on a carnival ride? I’m not lazy. I’m dizzy. And if meclizine lets me feed my cat without vomiting on her, then yes-I’ll take the foggy brain. You don’t get to romanticize recovery when you’ve never had your world spin sideways for 72 hours straight. Also, the dry mouth? I’ve chewed so much gum my dentist threatened to charge me extra.
Rusty Thomas
November 23, 2025 AT 00:41Meclizine is a government mind-control drug disguised as vertigo relief. They don’t want you to know the real cause-5G towers are messing with your inner ear fluid. I tested it. I went off meclizine for 3 days, turned on my WiFi router, and my head started spinning like a top. Took the pill again? Instant calm. Coincidence? I think not. Also, the FDA knows. They’re just scared of the truth. 🤫
Dave Wooldridge
November 23, 2025 AT 11:46They say ‘don’t mix with alcohol’-but what about kombucha? I had two sips and passed out on the couch. My wife said I snored like a chainsaw. Now I only drink it after 8 PM. And I only take meclizine at 10 AM. Timing is everything. Also, I think the FDA should require a warning label that says: ‘This pill will make you forget your own name.’ I forgot my dog’s name for 17 minutes once. He stared at me like I’d betrayed him.
Pawan Jamwal
November 25, 2025 AT 00:16Why are Americans so weak? In India, we take 3 tablets of meclizine and go to work. No one cares about drowsiness. You think your body is fragile? It’s not. It’s lazy. We have 100 million people with vertigo and not one of them is sitting home watching Netflix. You need discipline. Not a pill. Not therapy. Just grit. 🇮🇳💪
Bill Camp
November 26, 2025 AT 15:25My uncle took this for 11 years. Got dementia. Then he died. Coincidence? I don’t think so. Anticholinergics = brain rot. I’ve seen it. My cousin’s mom took it for motion sickness on road trips and now she can’t remember her kids’ birthdays. This isn’t medicine. It’s a slow poison wrapped in a blue pill. They’re selling you a trap and calling it relief.
Rebecca Cosenza
November 27, 2025 AT 05:22I don’t need a 1000-word essay to know this is dangerous. I took one pill. Felt like a zombie. Didn’t take another. Done. 🙃
Lemmy Coco
November 27, 2025 AT 16:34so i took meclizine for a week after my vestibular neuritis and it was a game changer… but then i tried to make coffee and forgot how to hold the mug. like… i just stared at it. my cat judged me. anyway. i switched to ginger tea and did the epley every morning. now i’m 90% better. no fog. no dry mouth. just me and my cat and a slightly less wobbly floor. also… typos are my love language.
rob lafata
November 28, 2025 AT 08:46You’re all missing the point. Meclizine isn’t the villain-it’s the symptom of a broken medical system. Doctors don’t have time to teach you vestibular rehab. So they hand out pills like candy. You’re not weak. You’re being exploited. And the pharma companies? They’re laughing all the way to the bank while you’re stuck in a fog, wondering why you can’t remember your kid’s name. This isn’t about vertigo. It’s about capitalism eating your brain. And nobody’s talking about it because they’re too busy Googling ‘how to stop dry mouth from meclizine.’
Matthew McCraney
November 28, 2025 AT 11:53My ex took this and became a completely different person. She stopped laughing. She forgot how to hug me. She said she felt ‘numb inside.’ I left her. Not because I didn’t love her-but because the pill stole her. And now she’s on a different drug. And I’m still alone. So yeah. I’m not just talking about side effects. I’m talking about soul erosion. And you think this is okay? You think this is medicine? It’s chemical abandonment.
serge jane
November 29, 2025 AT 06:39I’ve been on this for three years. I’m 71. I still walk my dog every morning. I still cook. I still laugh. I don’t believe in fear-based medicine. I believe in balance. The drug helps me live. The fear of it? That’s what kills people. Not the pill. The panic. The misinformation. The doctors who won’t listen. I read the studies. I talked to my pharmacist. I know the risks. And I still choose this. Because I choose to live. Not to survive. To live. And if that means a little fog? Fine. I’ve seen clearer skies.
Nick Naylor
November 30, 2025 AT 03:38According to the 2020 Cochrane meta-analysis (DOI: 10.1002/14651858.CD012854.pub2), meclizine demonstrates a statistically significant reduction in vertigo symptom severity (p<0.01) with a number needed to treat (NNT) of 2.8. However, the anticholinergic burden, particularly when combined with concomitant medications (e.g., SSRIs, antihypertensives), increases the risk of delirium by 3.2-fold in elderly populations (per Beers Criteria 2023). Additionally, prolonged use (>14 days) correlates with decreased vestibular compensation velocity (p=0.03). Clinical recommendation: limit to acute phase only. PT referral is mandatory. End of transmission.
Cinkoon Marketing
December 2, 2025 AT 02:26Just saying-if you’re taking this daily, you’re probably not doing the Epley maneuver right. Or you’re not doing it at all. I’ve seen so many people skip the rehab and just keep popping pills. It’s like taking ibuprofen for a broken leg. You’re not healing. You’re just hiding the pain. And then you wonder why you’re still dizzy. 🤷♀️