Why Proper Storage of Antibiotic Suspensions Matters
When your child is prescribed an antibiotic suspension, it’s not just about giving the right dose-it’s about keeping it effective. Liquid antibiotics for kids aren’t like pills. They’re mixed with water at the pharmacy, and once that happens, they start to break down. If stored wrong, they lose power. That means the infection won’t clear up, your child might get sicker, and bacteria could grow resistant to the medicine. The CDC found that 15% of pediatric antibiotic treatment failures are linked to improper storage. That’s not a small number. It’s one in seven kids who might not get better because the medicine wasn’t kept right.
Storage Rules Vary by Antibiotic
Not all liquid antibiotics are the same. Each one has its own rules. The most common one, amoxicillin, is forgiving. You can store it either in the fridge (2-8°C) or at room temperature (20-25°C). It stays good for 14 days either way. But here’s the catch: even though it’s okay at room temperature, many parents still refrigerate it because it tastes better cold. That’s fine-just don’t assume all antibiotics work the same way.
Amoxicillin/clavulanate (Augmentin) is different. It must be refrigerated. If left out, the clavulanate part breaks down fast. After just 5 days at room temperature, it loses nearly 10% of its strength. By day 10, it’s no longer reliable. So if your child’s prescription is Augmentin, the fridge isn’t optional-it’s required. And you must throw it away after 10 days, no exceptions.
Azithromycin (Zithromax) is the opposite. Never put it in the fridge. Cold temperatures make it thick and sticky. Kids hate it. Studies show it becomes 37% less palatable when chilled. It’s meant to be kept at room temperature and used within 10 days. The same goes for clarithromycin, clindamycin, sulfamethoxazole/trimethoprim, and cefdinir. These all lose effectiveness or become hard to swallow if cooled.
How Long Do These Suspensions Last?
Once mixed, every antibiotic suspension has a hard expiration date. This isn’t a suggestion-it’s science. Here’s what you need to know:
- Amoxicillin: 14 days, fridge or room temp
- Amoxicillin/clavulanate: 10 days, only in the fridge
- Azithromycin: 10 days, room temp only
- Other suspensions: Check the label-most are 7 to 14 days
Some parents think, “If it looks fine, it’s probably okay.” That’s dangerous. Even if the liquid looks clear and smells normal, potency drops over time. A 2023 study in the Journal of Pediatric Pharmacology and Therapeutics showed that amoxicillin/clavulanate loses over 15% of its active ingredient by day 11-even when refrigerated. That’s enough to let resistant bacteria survive.
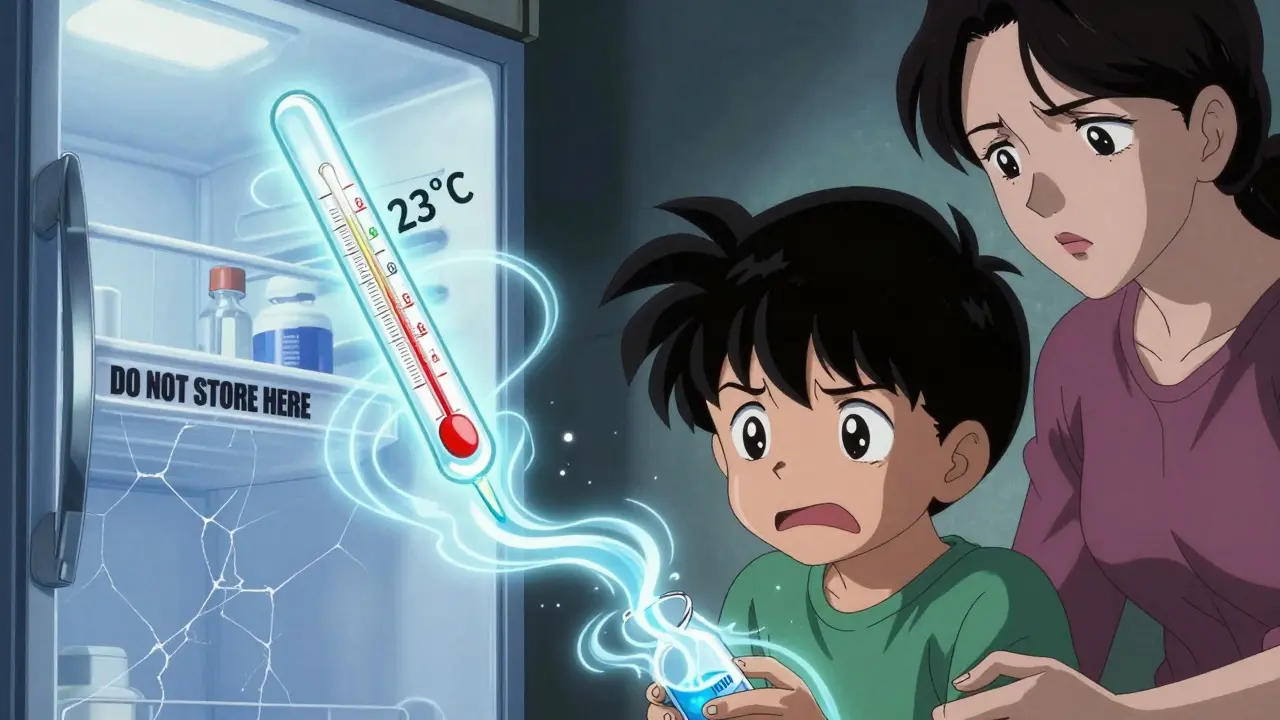
What Counts as “Room Temperature”?
Many people think “room temperature” means wherever the bottle sits on the counter. But in medical terms, room temperature is 20-25°C (68-77°F). In a hot kitchen, near a window, or in a bathroom with steam from the shower, it can easily hit 27-30°C (80-86°F). That’s too warm for most antibiotics. The FDA warns that 43% of households have temperatures above the safe range for medications.
Keep suspensions away from:
- Windowsills (sunlight heats them up)
- Stoves or ovens
- Bathroom cabinets (humidity and heat)
- Car glove compartments
Find a cool, dry spot-like a kitchen cabinet away from the stove, or a shelf in a bedroom. If your home gets hot in summer, consider moving the medicine to a cooler room.
Signs Your Antibiotic Has Gone Bad
You don’t need a lab test to tell if your suspension has spoiled. Look for these signs:
- Color change (yellowing, darkening, or cloudiness)
- Strange smell (sour, rancid, or chemical)
- Thickening or clumping (especially in azithromycin)
- Separation that won’t mix (shake the bottle-if chunks stay at the bottom, toss it)
- Changed taste (if your child says it tastes “off,” they’re probably right)
A 2023 survey of 2,543 parents found that 41% noticed discoloration, 37% noticed taste changes, and 22% saw sediment. If any of these happen, stop using it. Don’t guess. Call your pharmacist.
How to Remember When to Toss It
The biggest mistake? Keeping antibiotics past their discard date. The CDC says 37% of parents do this. Why? Because they forget.
Here’s how to fix it:
- Write the discard date on the bottle with a permanent marker as soon as you get it home.
- Ask the pharmacist to stick a “DISCARD BY” label on it. Most will do it if you ask.
- Set a phone reminder for the day before the expiration date.
- Put the bottle in a visible spot-not tucked away in a drawer.
One parent on Reddit said she used a mini-fridge just for her kids’ meds. Her treatment failures dropped from three in two years to zero. It’s not fancy, but it works.
What to Do With Expired or Unused Antibiotics
Never flush them down the toilet or throw them in the trash where kids or pets can reach them. The American Association of Poison Control Centers reports 60,000 accidental poisonings in kids under 5 every year from medications left within reach.
Use a drug take-back program. Many pharmacies, hospitals, or police stations have drop boxes. If that’s not available, mix the liquid with coffee grounds or cat litter in a sealed bag, then throw it in the trash. This makes it unappealing and unusable.
When in Doubt, Ask the Pharmacist
There’s a lot of conflicting advice online. Cleveland Clinic says amoxicillin can be stored at room temperature. MedlinePlus says it’s better refrigerated. The pharmacy label might say one thing, your pediatrician another. That’s confusing-and it’s why 52% of parents store antibiotics incorrectly.
The best rule? Check the label. If it says “Refrigerate,” refrigerate. If it says “Store at room temperature,” keep it out. If it’s unclear, call the pharmacy. Pharmacists are trained to know exactly what each suspension needs. They can also give you a new label with clear instructions. Don’t rely on memory or guesswork.
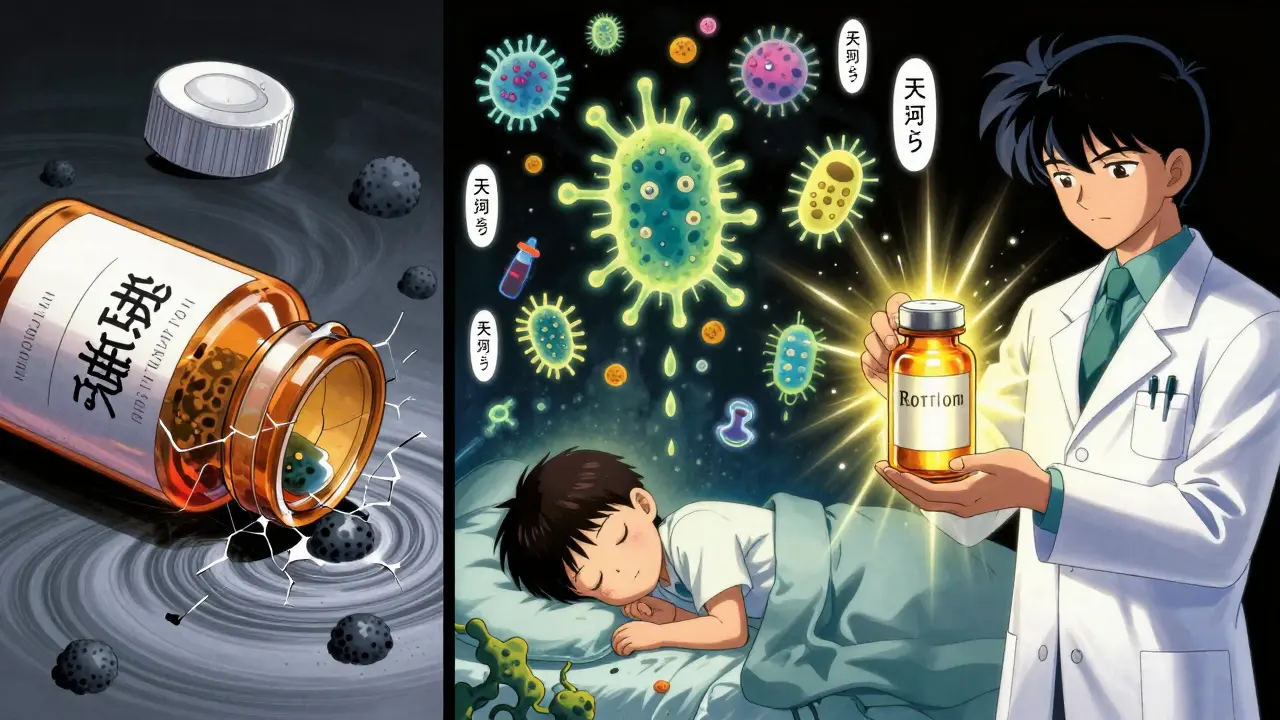
Why This Matters Beyond the Current Illness
Improper storage doesn’t just hurt your child this time. It helps create superbugs. When antibiotics are weak or incomplete, they don’t kill all the bacteria. The survivors multiply-and become resistant. That’s how we get MRSA, drug-resistant ear infections, and untreatable strep throat. The Infectious Diseases Society of America calls this one of the biggest threats to modern medicine.
Proper storage isn’t just about following rules. It’s about protecting your child’s health now-and the health of everyone in the future.


Dan Padgett
December 16, 2025 AT 01:41Man, I never realized how much science goes into this. I thought if it didn't look moldy, it was fine. Turns out, I've probably been giving my kid weak medicine for years. This post saved me from accidentally helping create a superbug. Thanks for laying it out like this.
Kayleigh Campbell
December 17, 2025 AT 08:34So amoxicillin’s chill at room temp but Augmentin turns into a science experiment if you don’t refrigerate it? Cool. So basically, the pharmacy is giving us a magic potion and we’re supposed to know which one needs to be kept in the icebox like a soda and which one’s fine on the counter like my expired hot sauce. I’m just glad I didn’t try to store it in the glove compartment.
Cassandra Collins
December 19, 2025 AT 02:10Wait… are you sure this isn’t a Big Pharma trick to sell more medicine? I read somewhere that the 10-day discard rule was made up so pharmacies could refill prescriptions faster. Also, why do they say not to flush it but then say mix it with cat litter? That’s just hiding it. They don’t want us to know what’s really in these bottles.
Randolph Rickman
December 20, 2025 AT 05:21This is exactly the kind of info every new parent needs. I wish I’d had this when my daughter had her first ear infection. I kept the azithromycin in the fridge because I thought cold = better. She wouldn’t take it for love or money. Turns out, it was just too thick. Lesson learned. Please share this with every mom group you know.
Kim Hines
December 20, 2025 AT 09:38I write the discard date on the bottle with a Sharpie now. Simple. Doesn’t need an app. Doesn’t need a reminder. Just look at it. Done.
sue spark
December 21, 2025 AT 10:29My kid hates the taste of antibiotics so I always chill them… I just found out I’ve been making azithromycin into glue for 3 years. I feel so dumb. But also… why does no one tell you this at the pharmacy? They just hand you the bottle and say ‘take it for 10 days’
Andrew Sychev
December 23, 2025 AT 01:1815% of treatment failures because parents are too lazy to read the label? That’s not a medical problem, that’s a parenting failure. You wouldn’t leave a baby seat in a hot car, so why leave medicine in the bathroom? If you can’t follow basic instructions, maybe don’t have kids.
Ron Williams
December 23, 2025 AT 02:12I’m from Nigeria and we don’t always have reliable fridges. We keep everything in the coolest corner of the house. I’m glad to know amoxicillin is okay at room temp. But I’ve been tossing out azithromycin after 7 days just to be safe. Better safe than sorry, right?
Arun ana
December 23, 2025 AT 18:26Wow, this is so helpful. I just got my daughter’s prescription and I was wondering why the pharmacist gave me two different labels. One said refrigerate, the other said room temp. Now I get it. I’m going to ask them to write the discard date on the bottle tomorrow. And I’ll put it on my fridge with a magnet. 🙌
Aditya Kumar
December 24, 2025 AT 19:25Too much info. I just give the medicine. If the kid gets better, it worked. If not, we go back. Done.
Tiffany Machelski
December 26, 2025 AT 17:25im gonna start using a mini fridge just for meds like that one mom said… sounds like a good idea… i think i saw one on amazon for like 50 bucks
Billy Poling
December 27, 2025 AT 21:59It is imperative to underscore that the integrity of pharmaceutical suspensions is contingent upon adherence to manufacturer-specified environmental parameters. Failure to comply with refrigeration protocols for beta-lactamase inhibitor combinations constitutes a violation of pharmacokinetic stability standards and may result in subtherapeutic serum concentrations, thereby increasing the likelihood of microbial selection pressure and the emergence of antimicrobial resistance. This is not a suggestion; it is a clinical imperative grounded in evidence-based pharmacology.