Running out of medication isn’t just inconvenient-it can be dangerous. But paying too much for prescriptions? That’s a quiet crisis millions face every year. Between rising drug prices, surprise co-pays, and forgotten refills, managing medication costs feels like juggling flaming torches. The good news? You don’t need a hospital budgeting team to take control. With the right tools and a simple system, you can set up medication budgeting and auto-refill alerts that save you money and stress.
Start by Tracking Every Prescription You Take
Before you can budget, you need to know what you’re spending. Write down every medication you take daily or weekly-name, dose, frequency, and where you fill it. Don’t forget over-the-counter drugs like insulin, inhalers, or blood pressure pills. These often get left out but add up fast.Use a free app like Medisafe or MyTherapy, or just a spreadsheet. Record the cost per refill and how often you refill it. For example:
- Metformin 500mg: $12 per 30-day supply, refilled monthly
- Albuterol inhaler: $45 per unit, refilled every 90 days
- Atorvastatin: $5 with insurance, refilled every 30 days
Do this for a full month. At the end, add it all up. That’s your baseline. If you’re spending $300 a month on meds, you now have a number to work with. No guesswork. No excuses.
Choose a Pharmacy That Works for Your Budget
Not all pharmacies charge the same. A $45 inhaler at Walgreens might cost $18 at Costco or Walmart’s $4 list. Some online pharmacies like Blink Health or GoodRx offer cash-price discounts that beat insurance. Use GoodRx or SingleCare to compare prices before you fill any prescription.Ask your pharmacist: “Is there a generic version?” or “Can I get a 90-day supply instead of 30?” Many insurers charge less for 90-day fills-sometimes half the cost. And if you’re on Medicare Part D, check your plan’s formulary. Some drugs are tiered, meaning you pay more if they’re not preferred. Switching to a preferred drug can cut your bill by 60%.
Set Up Auto-Refill Alerts That Actually Work
Most pharmacies offer auto-refill programs. But here’s the catch: they usually send alerts when your prescription is due to run out-not when you’re running low. That’s too late. You need alerts that trigger when you have 7-10 days left.Here’s how to make it work:
- Call your pharmacy and ask to enroll in auto-refill with early alerts.
- Set your alert to notify you 10 days before you run out.
- Turn on text or email alerts (don’t rely on phone calls-they get missed).
- Link your refill alerts to your calendar. Add a recurring event: “Check meds-refill if needed.”
Some apps like Medisafe and MyTherapy sync with your pharmacy and send alerts based on your actual usage. If you skip a dose, they adjust the refill date. That’s smarter than a rigid calendar. If you take your pills inconsistently, these apps adapt. Most are free.
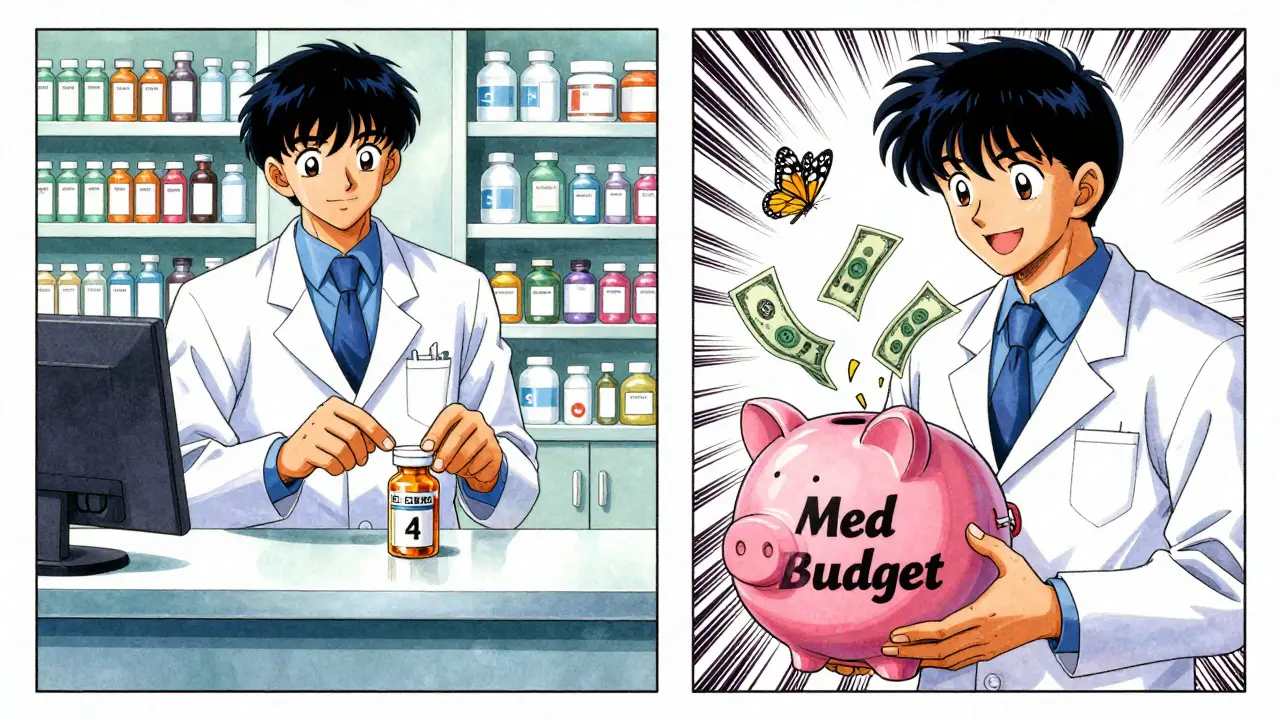
Create a Monthly Medication Budget
Now that you know your monthly spend, treat it like your rent or electric bill. Put it in your budget. If you spend $300 a month on meds, set aside $300 every payday. Don’t wait until the bill comes. That’s how people end up skipping doses to make ends meet.Use a separate savings account just for meds. Even $20 a week adds up to $1,040 a year. That’s enough to cover an unexpected price hike or a new prescription. If you’re on a fixed income, look into patient assistance programs. Most drug makers offer them. Pfizer, Merck, and AbbVie all have programs for low-income patients. You can apply online in 15 minutes.
Use Tech to Catch Price Changes Before They Hit You
Drug prices change often. A pill that cost $10 last month might jump to $25 this month. You won’t know unless you’re watching. Set up price alerts using GoodRx or RxSaver. These tools notify you when the cash price for your drug drops-or spikes.Some health systems now offer real-time pricing through their patient portals. If your doctor uses Epic or Cerner, check your portal. You might see a price estimate before you even leave the office. That’s huge. It lets you say, “Can we try a cheaper alternative?” before you get stuck with a $500 pill.
Watch for Generic Switches and Therapeutic Alternatives
When a brand-name drug loses its patent, generics flood the market. Prices drop by 80-90%. But your doctor might not know. If you’ve been on a drug for more than a year, ask: “Is there a generic now?”For example, the brand-name blood pressure drug Lisinopril-HCTZ used to cost $120 a month. The generic version? $4. That’s not a typo. Same pill. Same effect. But you have to ask. Pharmacies often don’t switch you automatically.
Some apps like Medisafe flag when a drug you take has gone generic. Others connect to your pharmacy’s formulary and suggest cheaper alternatives with the same effect. That’s called therapeutic interchange. It’s common in hospitals. Now it’s available to you.
What to Do When You Can’t Afford a Prescription
If you’re skipping doses because of cost, you’re not alone. One in four Americans says they’ve skipped a medication due to price. But there are options.- Ask your doctor for samples. Many still have them.
- Apply for a patient assistance program. You need proof of income, but it’s usually fast.
- Check NeedyMeds.org. It’s a free database of discount programs for every major drug.
- Call your pharmacy’s social worker. Many have them on staff.
Don’t wait until you’re sick. Act before you run out. One missed dose of insulin or blood pressure meds can land you in the ER-and cost you thousands.
Keep It Simple. Keep It Going.
You don’t need fancy software. You don’t need a team. You need three things:- A list of your meds and their costs.
- Auto-refill alerts set for 10 days before you run out.
- A dedicated fund for meds, paid on payday.
Check in once a month. Did your price go up? Did you miss a refill? Did a generic become available? Adjust. That’s all. The goal isn’t perfection. It’s consistency. Small steps, repeated, change everything.
People who do this cut their medication costs by 20-40% in the first year. Not because they’re rich. Not because they’re smart. Because they took control.
Can I set up auto-refill alerts without a smartphone?
Yes. Most pharmacies allow you to enroll in auto-refill by phone. Call your pharmacy, ask to be enrolled, and request text or email alerts. If you don’t have a smartphone, ask for a paper reminder card or a phone call reminder. Many pharmacies still offer this service, especially for seniors.
Do auto-refill alerts work with Medicare Part D?
Yes. Medicare Part D plans work with most pharmacies to offer auto-refill. You’ll still pay your plan’s copay, but you won’t risk running out. Some plans even offer free shipping on auto-refills. Check your plan’s website or call member services to enroll.
What if my insurance doesn’t cover my medication anymore?
Don’t panic. First, ask your doctor if there’s a covered alternative. If not, use GoodRx to find the lowest cash price. Then apply for a patient assistance program through the drug manufacturer. Many companies offer free or low-cost meds to people who qualify based on income. You can apply online in under 10 minutes.
How do I know if a generic drug is safe?
All generics approved by the FDA must contain the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They’re tested to be bioequivalent-meaning they work the same way in your body. The only differences are inactive ingredients, like fillers or dyes, which rarely affect effectiveness. If you’ve had no reaction to the brand, you’ll likely have no reaction to the generic.
Is medication budgeting only for people with many prescriptions?
No. Even if you only take one or two meds, the cost can be high. A single specialty drug like Humira can cost over $7,000 a month. Budgeting helps anyone who pays for prescriptions. The system scales-whether you spend $10 or $1,000 a month.
Can I use this system if I’m on Medicaid?
Absolutely. Medicaid often covers most prescriptions at low or no cost. But prices can still vary between pharmacies. Use GoodRx to compare cash prices-sometimes the cash price is lower than your Medicaid copay. Auto-refill alerts help you avoid lapses in coverage, which can lead to denied refills or higher costs later.


Darren McGuff
January 10, 2026 AT 09:37Love this breakdown. I’ve been using GoodRx for my dad’s statins and saved $110/month. The cash price was lower than his Medicare Part D copay-shocking, but true. Set up auto-refill via phone last month, got a text alert 10 days out. No more panic runs to the pharmacy at 7 PM on a Sunday. Simple. Free. Life-changing.
Pro tip: Call your pharmacy and ask if they’ll hold your refill for a week if you’re traveling. They’ll usually say yes if you’re a regular.
Also, never assume your insurance covers it. Always check the price before you walk out the door. I’ve been burned twice. Never again.
Kiruthiga Udayakumar
January 11, 2026 AT 00:42As someone from India who’s watched my mom skip doses because insulin cost more than her monthly groceries, this hit hard. The US system is broken, but your tips? Universal. We use WhatsApp reminders here since phones are everywhere-even without smartphones. My mom gets a daily text: ‘Take pill.’ Simple. But it works.
Also, generic drugs? Same active ingredient. Same results. The color’s different, sure. But your kidneys don’t care if it’s blue or white. Stop being scared of generics. They’re not ‘cheap’-they’re smart.
Ashley Kronenwetter
January 11, 2026 AT 13:38While the intent of this guide is commendable, the assumption that all individuals have access to smartphones, internet, or even reliable transportation to compare pharmacy prices is deeply flawed. Many elderly, rural, and low-income populations rely on community clinics and mail-order services. The suggestion to ‘call your pharmacy’ presumes phone access, consistent hours, and patient advocacy skills-privileges not universally held. A more equitable framework would include state-funded medication navigation programs, not just individual hustle.
Micheal Murdoch
January 13, 2026 AT 05:35There’s a quiet dignity in managing your own health like this-not because you’re ‘responsible,’ but because the system won’t do it for you. I used to skip my blood pressure meds when the copay jumped to $80. Then I started tracking. Found out my 30-day supply was $12 at Walmart. I switched. Set up a text alert. Now I refill every 28 days, not 30, just to be safe.
It’s not about being perfect. It’s about being stubborn enough to keep showing up for yourself. One pill at a time. One dollar saved at a time.
And yes, generics are safe. I’ve been on them for 8 years. My doctor didn’t even tell me they switched me. I found out when I checked the bottle. Didn’t feel any different. Didn’t need to.
Small steps. Big results. You don’t need a budgeting app. You just need to care enough to look.
Ian Long
January 14, 2026 AT 18:49Just want to say thank you. I’ve been on Humira for 5 years. $7,000/month. I cried the first time I found a patient assistance program that covered 90% of it. Took me 6 months to apply. Didn’t know where to start. This guide? It’s the kind of thing I wish I’d had back then.
Also-yes, your insurance can drop coverage overnight. I had that happen. Called my doctor. They had samples. Got me through 3 weeks until the new plan kicked in. Don’t be ashamed to ask. We’re all just trying not to die here.
Chris Kauwe
January 15, 2026 AT 03:47Let’s be real: this isn’t ‘budgeting.’ It’s survival theater. The system is designed to extract wealth from the sick. You’re not ‘taking control’-you’re playing a rigged game with a single life raft. The fact that you need to ‘set alerts’ and ‘compare prices’ to avoid dying is not empowerment. It’s systemic failure dressed up as self-help.
But hey, if you want to feel good about your 20% savings while millions still skip doses? Go ahead. I’ll be here, watching the pharmaceutical CEOs buy their third vacation homes.
Heather Wilson
January 16, 2026 AT 14:04Why are you all acting like this is revolutionary? I’ve been doing this since 2017. You don’t need an app. You don’t need a spreadsheet. You need a notebook. Write down your meds. Write down the cost. Call the pharmacy. Ask for the cash price. Write it down. Do this once a month. That’s it.
And yes, generics work. I took a brand-name antidepressant for 3 years. Switched to generic. Same pill. Same results. My therapist didn’t even notice. The only difference? My bank account didn’t cry.
Stop overcomplicating it. People die because they think this is too hard. It’s not. It’s just inconvenient. And inconvenience is the price of not being rich.
Patty Walters
January 17, 2026 AT 13:39OMG YES. I just switched to the generic for my thyroid med and saved $60 a month. I didn’t even know it was possible until I read this. I use Medisafe and it’s so easy. I used to forget to refill and then panic. Now I get a text and I’m like ‘oh right, time for my pills again.’
Also, I have no smartphone but I use my daughter’s old flip phone to get texts. They still work. Just ask your pharmacy to send texts to a basic phone. They’ll do it. I did.
Also, GoodRx is a lifesaver. I just wish more people knew about it.
Matthew Maxwell
January 19, 2026 AT 06:12It is both a moral failure and a personal dereliction of duty to allow one’s health to be subject to the whims of corporate pricing structures. One must not merely ‘track’ medications- one must cultivate a disciplined, almost monastic vigilance over one’s own biological integrity. The notion that a ‘$4 inhaler’ is a victory is a tragic testament to the collapse of civic responsibility. The true solution lies not in app-based alerts, but in the reclamation of medical sovereignty through systemic reform-of which your casual, consumerist advice is but a Band-Aid on a hemorrhaging artery.