Glaucoma doesn’t shout. It doesn’t cause pain or blurry vision in the early stages. By the time you notice something’s wrong, the damage is often permanent. That’s why it’s called the silent thief of sight. Around 76 million people worldwide have it today, and that number is expected to climb to over 110 million by 2040. Most don’t know they have it until it’s too late.
What Actually Happens in Glaucoma?
At its core, glaucoma is damage to the optic nerve-the cable that sends visual information from your eye to your brain. This damage isn’t random. It’s usually tied to pressure inside the eye, called intraocular pressure (IOP). Normal IOP ranges from 10 to 21 mmHg. Anything above that raises your risk. But here’s the twist: not everyone with high pressure gets glaucoma, and not everyone with glaucoma has high pressure.
The real culprit is mechanical strain at the back of the eye, where the optic nerve exits. A mesh-like structure called the lamina cribrosa acts like a sponge-like barrier. When pressure builds up, this structure gets stretched. Studies show that in glaucoma patients, this area moves backward 30-50% more than in healthy eyes. That constant tugging damages the nerve fibers passing through it. These fibers are part of retinal ganglion cells, and once they die, they don’t come back.
It’s not just about pressure inside the eye. Your brain’s pressure-called intracranial pressure (ICP)-also matters. Think of it like water pressure in a hose. If the pressure outside the hose is low and the pressure inside is high, the hose bursts. In glaucoma, if your eye pressure is 20 mmHg and your brain pressure is only 10 mmHg, that 10-point difference is pulling on the optic nerve. That’s why some people with IOP under 15 mmHg still lose vision. This is called normal-tension glaucoma, and it’s especially common in Asian populations, making up nearly half of all glaucoma cases there.
Types of Glaucoma: It’s Not Just One Disease
There are several types, and each behaves differently.
Primary open-angle glaucoma (POAG) is the most common-about 90% of cases in the U.S. The drainage system in your eye slowly clogs over time. Fluid builds up. Pressure rises. You feel nothing. This form creeps up silently, often after age 50.
Normal-tension glaucoma (NTG) is the puzzling one. IOP stays below 21 mmHg, yet the optic nerve still gets damaged. Studies show that reducing IOP by just 30% in NTG patients cuts progression risk from 35% to 12% over seven years. That proves pressure-even if it’s "normal"-still matters. Some researchers believe poor blood flow to the optic nerve or autoimmune issues might be at play here.
Angle-closure glaucoma is less common globally but far more dangerous. It happens when the iris blocks the drainage angle suddenly. Pressure spikes fast-sometimes to 40 or 50 mmHg. Symptoms include severe eye pain, headache, nausea, and seeing halos around lights. This is an emergency. Without treatment, you can lose vision in days.
Secondary glaucomas come from other problems: eye injuries, inflammation, tumors, or even long-term steroid use. Pseudoexfoliative glaucoma, where flaky material clogs the drainage system, is especially aggressive and common in older adults.
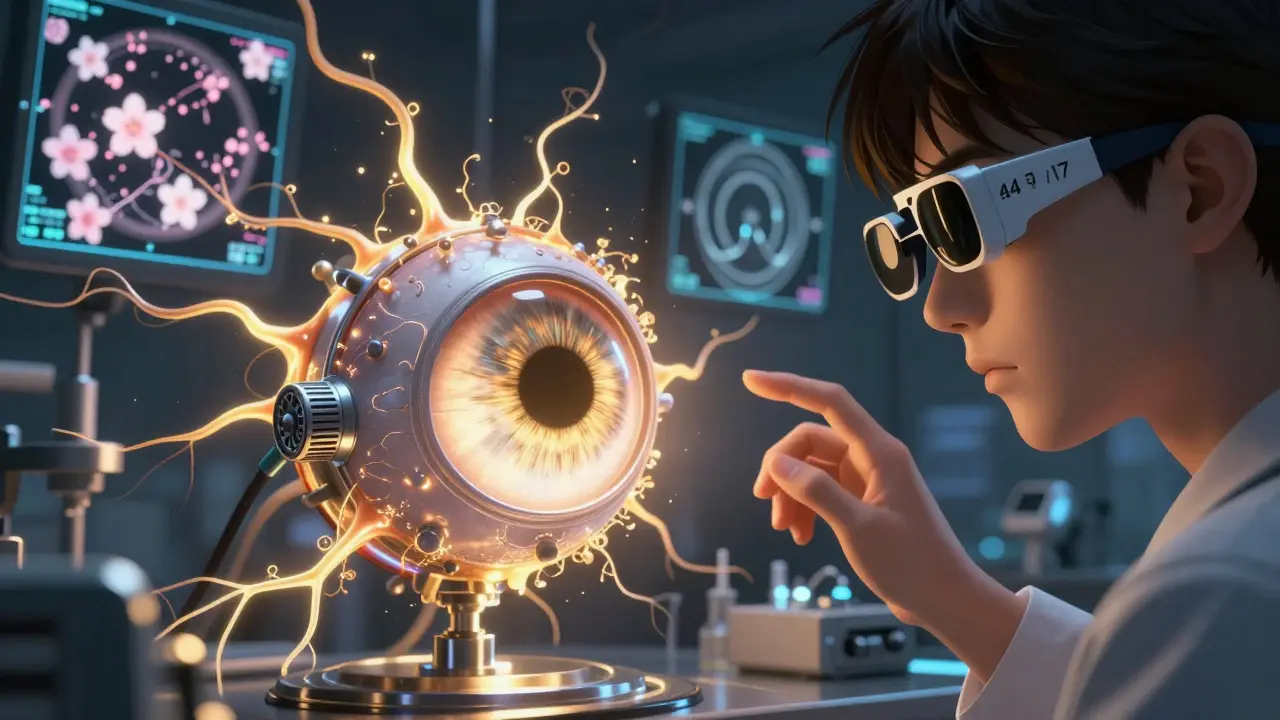
How Do Doctors Diagnose It?
Since glaucoma shows no early symptoms, diagnosis relies on tools-not how you feel.
- Tonometry measures eye pressure. The gold standard is Goldmann applanation tonometry. It’s accurate, but pressure changes throughout the day-highest in the morning. That’s why a single reading can be misleading.
- Optical Coherence Tomography (OCT) takes ultra-detailed images of the optic nerve and retinal nerve fiber layer. It can detect thinning as small as 5-10 microns-thinner than a human hair. This is often the first sign of damage.
- Visual field testing (like Humphrey perimetry) checks your peripheral vision. It finds blind spots as small as 1 dB in sensitivity. Glaucoma eats away at your side vision first, so you won’t notice until it’s advanced.
- Fundus photography captures images of the optic disc. A larger cup-to-disc ratio means more nerve loss.
Doctors combine these tests. One alone isn’t enough. A person might have high pressure but a healthy optic nerve. Another might have normal pressure but clear nerve damage on OCT. Both need treatment.
Treatment: Lowering Pressure Saves Sight
The goal isn’t to cure glaucoma-it’s to stop it from getting worse. And the most proven way is lowering IOP.
Eye drops are the first line. Prostaglandin analogs like latanoprost reduce pressure by 25-33% with just one drop a day. But side effects are real: eyelashes grow longer, eyelids darken, and fat around the eyes can sink in. About 1 in 5 people stop taking them because of this.
Laser treatment (trabeculoplasty) opens up the drainage system. It works in 75% of cases at first, but effectiveness drops about 10% each year. It’s not a cure, but it can delay the need for surgery.
Surgery is for advanced cases. Trabeculectomy creates a new drainage channel. It’s 85-90% successful in the first year, but many scar over time. Newer options like MIGS (minimally invasive glaucoma surgery), such as the iStent, are safer and faster. They lower pressure by 20-25%, with 70-80% success at two years.
Target pressure isn’t one-size-fits-all. If you have mild glaucoma, doctors might aim for 18-21 mmHg. For severe cases, they’ll push it down to 12-15 mmHg. That’s a 30-50% drop from your baseline. The Early Manifest Glaucoma Trial showed that hitting this target cuts progression risk by half.
Why People Stop Treatment-and What Happens When They Do
Here’s the ugly truth: half of glaucoma patients stop their eye drops within a year. Only 25% are still using them after two years.
Why? Side effects. Forgetting. Cost. And the fact that they feel fine. If you don’t see changes, it’s easy to think, "It’s not working," or "I don’t need it anymore." But glaucoma doesn’t care how you feel. It keeps damaging your nerve fibers quietly.
A 2022 survey of 1,200 patients found 68% lived in fear of blindness. That anxiety is real. But the data shows: those who stick with treatment rarely lose vision. One patient on a forum wrote that after a trabeculectomy, their pressure dropped from 32 to 14 mmHg-and their vision stabilized for over 10 years. That’s the power of consistent care.
The Future: Beyond Pressure Lowering
Researchers are no longer just focused on pressure. They’re looking at ways to protect the nerve itself.
One promising area is neuroprotection. The drug brimonidine, originally used to lower pressure, may also directly protect nerve cells. In the LIBERTI study, NTG patients on brimonidine had 30% slower vision loss than those on timolol-even when pressure was equally low.
Other experiments are even more exciting. Oncomodulin, a natural growth factor, has triggered 40% axon regeneration in animal studies. CNTF implants (a nerve growth protein) preserved 2.5 dB more vision over two years in early trials. Gene therapy is being tested to fix the drainage system at the root level-early results show 25% IOP reduction in six months.
Home monitoring is also coming. Contact lenses like the Triggerfish sensor track pressure 24/7, with accuracy within 1.5 mmHg. AI-powered OCT analysis can now detect early glaucoma with 94% accuracy. These tools could make diagnosis faster and treatment more personal.
What You Can Do
If you’re over 40, get your eyes checked-even if you see fine. If you have a family history, start even earlier. Glaucoma runs in families. If you’re African, Hispanic, or Asian, your risk is higher.
Don’t wait for symptoms. If you’re diagnosed, take your drops every day. Set phone reminders. Talk to your doctor about side effects-there are alternatives. If your pressure is normal but you have nerve damage, don’t assume you’re safe. You still need treatment.
Glaucoma isn’t a death sentence. It’s a chronic condition, like high blood pressure. Manage it, and you keep your sight. Ignore it, and you risk losing it forever.
Can glaucoma be cured?
No, glaucoma cannot be cured. Once retinal ganglion cells die, they don’t regenerate. But with early detection and consistent treatment, progression can be stopped or slowed dramatically. Most people who follow their treatment plan keep their vision for life.
Is high eye pressure always glaucoma?
No. Having high eye pressure (ocular hypertension) means you’re at higher risk, but not everyone with it develops glaucoma. About 10% of people with pressure over 21 mmHg will develop optic nerve damage over 10 years. Regular monitoring is key to catching damage early.
Can I have glaucoma with normal eye pressure?
Yes. This is called normal-tension glaucoma (NTG). It accounts for 20-30% of cases in Western countries and up to 70% in parts of Asia. Damage occurs even when pressure stays below 21 mmHg. The cause may involve poor blood flow, low intracranial pressure, or genetic factors. Treatment still focuses on lowering IOP by 30% or more to slow progression.
How often should I get tested for glaucoma?
If you’re over 40 with no risk factors, get a comprehensive eye exam every 2-4 years. If you’re over 60, every 1-2 years. If you have a family history, diabetes, or are African or Asian descent, start screening at 35 and get checked every 1-2 years. Once diagnosed, follow-up tests (IOP, OCT, visual field) are usually every 3-12 months.
Do glaucoma eye drops have long-term side effects?
Yes. Prostaglandin analogs like latanoprost can cause permanent darkening of the iris, longer eyelashes, and sunken eyes due to fat loss around the socket. Beta-blockers like timolol can lower heart rate and cause breathing issues in people with asthma. If side effects bother you, talk to your doctor. Newer drops and combination therapies are available with fewer side effects.
Can lifestyle changes help with glaucoma?
Lifestyle won’t cure glaucoma, but it can help. Regular aerobic exercise (like brisk walking) lowers IOP by 10-20% for a few hours. Avoid inverted yoga poses, which raise eye pressure. Don’t smoke-nicotine reduces blood flow to the optic nerve. Eat leafy greens and omega-3s; some studies link them to lower risk. But none of this replaces medication or monitoring.

Philip House
January 22, 2026 AT 08:19Look, I’ve read every paper on this. Glaucoma isn’t even a real disease-it’s just the medical-industrial complex selling drops to people who don’t need them. I’ve had IOP at 24 for 12 years. No damage. No symptoms. They’re scaremongering to sell prostaglandins. Your brain pressure? Nobody measures that. It’s all guesswork.
And don’t get me started on OCT. It’s a $200k machine that tells you what your grandma’s eye exam already could. We’re overdiagnosing normal aging as pathology. Wake up, people.
Ryan Riesterer
January 23, 2026 AT 09:04The biomechanical strain hypothesis at the lamina cribrosa is well-supported by in vivo OCT elastography studies (e.g., Liu et al., 2021). The 30–50% posterior displacement in glaucomatous eyes correlates strongly with axonal transport disruption, not merely IOP elevation.
Normal-tension glaucoma (NTG) exhibits significantly lower translaminar pressure gradient (IOP–ICP) values, consistent with the hydraulic hypothesis. Intracranial pressure averaging 10–12 mmHg in NTG patients-versus 15–18 mmHg in controls-creates a net pressure differential sufficient to induce axonal shearing, even with IOP <18 mmHg.
Akriti Jain
January 23, 2026 AT 19:34So… you’re telling me Big Pharma doesn’t want us to know that eye pressure is controlled by the moon phases? 🌕👁️
My cousin in Delhi had glaucoma after using her iPhone for 12 hours straight. The doctor said ‘it’s genetic.’ LMAO. I say it’s 5G + fluoride in the water. They’re testing this on brown people first. 🤡
Also, I’ve been applying coconut oil to my eyelids since 2021. My IOP dropped to 8. Coincidence? I think not. #GlaucomaIsACult
Mike P
January 24, 2026 AT 14:53Y’all are overcomplicating this. Glaucoma? It’s just your eyes saying ‘I’m tired of this BS.’ You’re sitting in front of screens all day, drinking soda, and thinking eye drops are gonna fix it?
I used to have pressure at 26. Stopped the drops. Started doing push-ups every morning. Walked 10k steps. Cut out sugar. My pressure’s at 15 now. No meds. No lasers. Just American grit.
And if you think a $5000 OCT machine is better than a good ol’ eye chart? You’re part of the problem. We don’t need tech-we need discipline. Get off your couch. Stop blaming doctors. Take responsibility.
Also, your ‘normal’ pressure? Probably just low blood pressure. You’re anemic. Eat more steak. Problem solved.
Jasmine Bryant
January 25, 2026 AT 12:57Wait, so if I have NTG and my IOP is 14, but my ICP is 11, that means the pressure difference is 3 mmHg? That seems really low to cause damage…
Also, I read somewhere that sleep apnea can lower ICP-could that be why some people with NTG have worse progression? I think I saw a study linking it… but I can’t find it again. Anyone know the citation?
And I’ve been using my phone to remind me to take drops, but sometimes I forget if I’m in the shower. Any tips? I feel so guilty when I miss a day 😅
Liberty C
January 26, 2026 AT 05:02How is it possible that you’re still trusting the same outdated, 19th-century paradigm of ‘pressure = damage’? You’re clinging to a model that was debunked by neuroscientists in 2007.
Glaucoma is a neurodegenerative disorder, period. The eye is just the battlefield. The real issue? Chronic systemic inflammation, mitochondrial dysfunction, and yes-your soul’s disconnection from cosmic energy. You think eye drops fix that? Please. You’re treating symptoms like a child slapping a bandage on a severed artery.
Try fasting. Try breathwork. Try chanting mantras at 4 AM while staring at a candle. Your optic nerve will thank you. Not the ophthalmologist. You. The one who dares to think beyond the pill bottle.
shivani acharya
January 27, 2026 AT 04:48Oh, so now it’s not just Big Pharma-it’s also the government, the WHO, the WHO’s secret shadow branch, and the Chinese lab that invented the tonometer? I’ve been waiting for someone to say it out loud.
My uncle in Mumbai had glaucoma. He took drops for 8 years. Then one day, he stopped. Ate turmeric, slept on his left side, and cried into a bowl of mangoes. His pressure dropped to 11. No damage. No surgery. They called it ‘spontaneous remission.’ I call it a cover-up.
And don’t even get me started on OCT. That machine is just a fancy camera that scans your soul. They’re collecting your eye data to sell to advertisers. ‘You looked at a green screen for 4.2 seconds. You’re probably depressed. Here’s a coupon for latanoprost.’
They’re not curing glaucoma. They’re creating it. To keep you dependent. To keep you afraid. To keep you buying.
And if you think exercise helps? That’s what they want you to believe. So you don’t ask questions. So you don’t realize the truth: glaucoma is a psyop. The real enemy? The mirror. You’re seeing your own fear in your pupil. That’s what’s killing you.
Wake up. The drops are poison. The machines are lies. The truth? You’re being watched. Even now. Right now. Through your eyes.
Sarvesh CK
January 29, 2026 AT 01:52It is fascinating how the understanding of glaucoma has evolved from a purely mechanical model of intraocular pressure to a complex interplay of biomechanical, vascular, and neurodegenerative factors.
The concept of the translaminar pressure gradient-differential pressure across the lamina cribrosa-offers a compelling unifying framework that reconciles both high-tension and normal-tension forms. This suggests that the optic nerve head is not merely a passive structure subjected to pressure, but an active biological interface sensitive to microenvironmental homeostasis.
Moreover, the regional variations in prevalence, particularly the higher incidence of normal-tension glaucoma in East Asian populations, may reflect genetic polymorphisms in genes related to cerebrospinal fluid dynamics or extracellular matrix composition. Future research must integrate genomics, biomechanics, and neuroimaging to develop truly personalized interventions.
It is also worth noting that the psychological burden of chronic, asymptomatic disease often leads to non-adherence, not from negligence, but from the existential dissonance of treating something one cannot perceive. Empathy in patient care may be as vital as IOP reduction.
Hilary Miller
January 30, 2026 AT 21:49My grandma in Lagos had glaucoma. No drops. No doctor. Just mango leaves and prayer. She saw till she was 98.
Don’t forget: culture matters. In some places, ‘eye pressure’ is just a word. What matters is whether you can still see your child’s face.
Check your eyes. Not because the world says so. Because you love life.