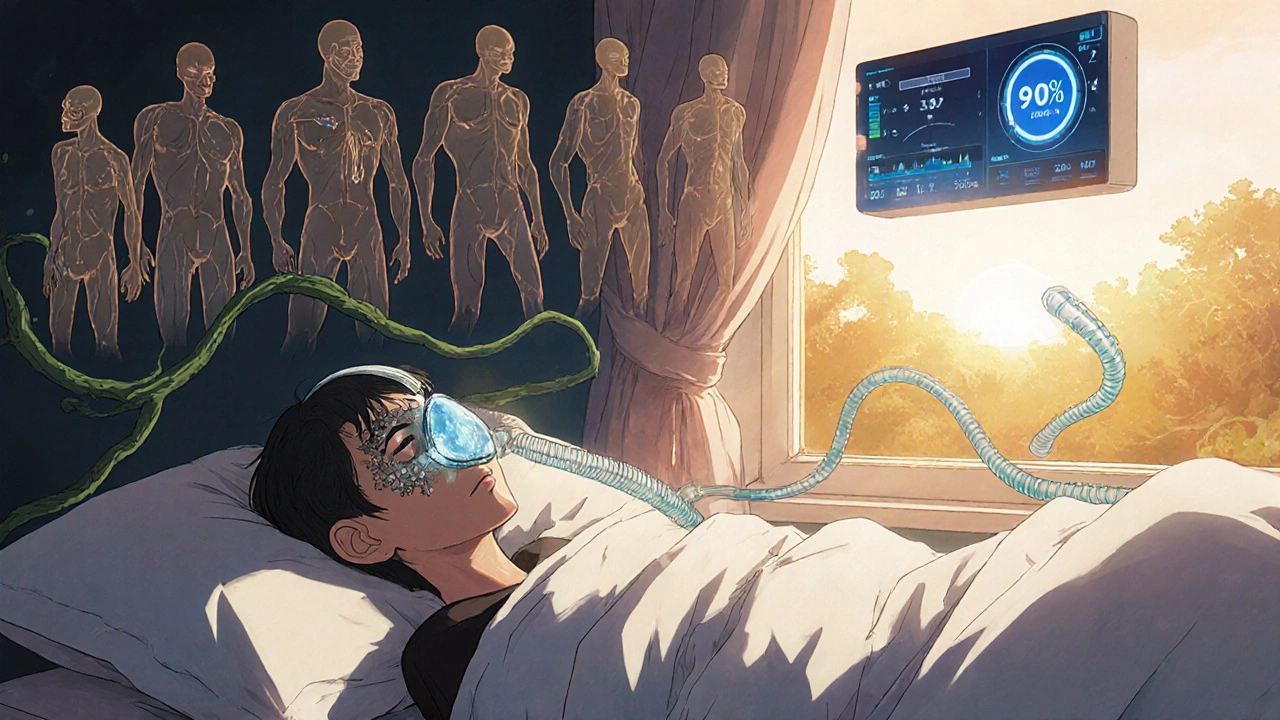
Why Your CPAP Isn’t Working (And How to Fix It)
You bought the CPAP machine. You followed the setup instructions. You’re using it every night. But you still wake up with a dry mouth, your mask keeps leaking air, and the pressure feels like it’s crushing your chest. You’re not alone. About 42% of CPAP users deal with dry mouth, 58% struggle with mask leaks, and 31% say the pressure feels wrong. These aren’t rare problems-they’re the main reasons people quit therapy. The good news? Most of these issues have simple, proven fixes.
Dry Mouth? It’s Probably Not the Humidifier
Most people blame their CPAP humidifier when they wake up with a parched throat. But here’s the truth: dry mouth is almost always caused by mouth breathing, not low humidity. If you’re breathing through your mouth while sleeping, the pressurized air from your CPAP escapes out of your mouth instead of staying in your airway. That’s what dries you out.
Here’s how to fix it:
- Try a chin strap. This simple device holds your jaw closed so you breathe through your nose. 45% of mouth breathers who use one report dry mouth disappearing within days.
- Switch to a full-face mask. These cover both your nose and mouth. One Reddit user, u/SleepSeeker2020, said his dry mouth vanished after switching from a nasal mask to a full-face mask in just three nights.
- Adjust your humidifier. Set it to level 3 or 4 on a 0-6 scale. Too low? Your air stays dry. Too high? You get condensation in the tube (rainout). Most users find level 3-4 hits the sweet spot.
- Use heated tubing. It keeps the air warm as it travels from the machine to your mask, reducing moisture loss. Philips’ 2022 trial showed heated tubing cuts dry mouth by 32%.
Don’t just crank up the humidity. Fix the root cause: mouth breathing.
Mask Leaks? It’s Usually the Fit, Not the Machine
A leaking mask doesn’t just waste air-it makes your therapy less effective. Dr. David White, a leading sleep specialist, says leaks over 24 L/min significantly reduce treatment results. You might hear a hissing sound, wake up with red marks, or see high leak readings on your machine’s app.
Here’s how to fix leaks without buying a new mask:
- Check the cushion. If it’s cracked, stiff, or discolored, replace it. DME providers recommend replacing mask cushions every 3 months.
- Adjust the headgear. Too tight? You’ll get pressure sores. Too loose? Air escapes. The right fit is snug but not painful. Try this trick: With your CPAP running, gently pull the mask away from your face until you hear air hissing. Then slowly push it back until the noise stops. That’s your seal.
- Don’t over-tighten. Many users crank the straps too hard thinking it’ll stop leaks. That actually distorts the cushion and makes leaks worse.
- Try a different mask style. If you’re using a nasal pillow and it leaks, try a nasal mask. If you’re using a nasal mask and still leaking, try a full-face mask. Mask fit is personal.
One survey of 1,247 CPAP users found 72% solved their leaks just by adjusting headgear straps. No new equipment needed.

Pressure Too High? Too Low? Here’s How to Tell
CPAP pressure is set between 4 and 25 cm H₂O. Most people start around 8-10 cm H₂O. But if your pressure feels too high, you might feel chest pressure, have trouble exhaling, or wake up gasping. If it’s too low, you’ll still snore or feel like you’re not getting enough air.
Here’s what to look for:
- Too high: Chest discomfort, bloating, dry mouth, difficulty falling asleep.
- Too low: Snoring, waking up tired, AHI (apnea-hypopnea index) readings above 5 on your machine’s app.
Dr. Nancy Collop from Johns Hopkins says pressure settings below 5 cm H₂O can still be effective for many people-especially if they’re mild sleep apnea cases. But here’s the catch: you shouldn’t adjust pressure yourself. Most machines let you tweak it by ±2 cm H₂O, but going beyond that voids your warranty and can be unsafe.
Instead:
- Check your machine’s data. Most modern CPAPs (like ResMed AirSense 11 or Philips DreamStation 2) track your AHI and leak rates nightly. If your AHI is above 5 after two weeks, talk to your sleep doctor.
- Ask about expiratory pressure relief (EPR). This feature lowers the pressure slightly when you breathe out. One Reddit user, u/ExhaustedEngineer, went from 14 cm H₂O (which caused chest pain) to 9 cm H₂O with EPR turned on-and slept better than ever.
- Consider an auto-adjusting (APAP) machine. These respond to your breathing in real time, adjusting pressure every 5-10 seconds. ResMed’s AutoSet algorithm gets 4.2/5 stars for comfort; Philips DreamStation gets 3.8/5.
Never guess your pressure. Let your sleep specialist use your machine’s data to make the call.
What Machines Handle These Problems Best?
Not all CPAPs are created equal. Here’s how the top models handle dry mouth, leaks, and pressure:
| Model | Dry Mouth Help | Leak Detection | Pressure Adjustment | Noise Level |
|---|---|---|---|---|
| ResMed AirSense 11 | Heated tubing + ClimateControl humidifier | Detects leaks as low as 12 L/min | AutoSet algorithm (smart pressure changes) | 25-27 dB |
| Philips DreamStation 2 | Humidification + heated tube | Good detection, but less precise | AutoRamp + SmartStart | 26-28 dB |
| Fisher & Paykel SleepStyle | Simple humidifier, no heated tube | Basic leak alerts | Fixed pressure only | 28-30 dB |
The AirSense 11 leads in leak detection and smart pressure, making it the best for users who struggle with leaks or variable breathing. DreamStation 2 is a solid second, especially if you use the DreamMapper app for personalized tips. SleepStyle is cheaper but lacks advanced features.
When to Call Your Sleep Doctor
You can fix most CPAP issues on your own. But if you’ve tried the fixes above and still feel awful, it’s time to call your sleep specialist. Here’s when:
- Your AHI stays above 5 after 2-4 weeks of consistent use.
- You have persistent dry mouth even with a chin strap and heated tubing.
- Your mask leaks more than 24 L/min despite trying different sizes and styles.
- You feel claustrophobic or anxious every time you put the mask on.
- You’re using the machine less than 4 hours a night.
Your doctor can re-titrate your pressure, recommend a different mask, or check for other issues like nasal congestion or allergies. Don’t wait until you quit therapy. A quick 15-minute call can save months of frustration.
Keep Your Machine Running Smoothly
A dirty CPAP is a broken CPAP. Maintenance is the secret to long-term success.
- Wash your mask cushion and headgear daily with mild soap and water.
- Replace the filter every 30 days for foam, every 90 days for HEPA.
- Empty and dry the water chamber every morning. Don’t let water sit overnight.
- Replace tubing every 6 months, or sooner if you see cracks.
ResMed’s 2023 data shows 89% of users who follow these steps report fewer issues and better sleep. It’s not glamorous-but it works.
Why Most People Quit (And How to Avoid It)
Only 46% of CPAP users meet the Medicare standard of 4+ hours per night. Why? The first two weeks are brutal. You feel awkward. You wake up with a dry mouth. Your mask leaks. You hate it.
But here’s the data: 78% of users who stick with it for 14 days report major improvements. The discomfort fades. The benefits kick in: better sleep, clearer thinking, lower blood pressure.
Don’t give up after a bad night. Give it two weeks. Use a chin strap. Adjust your humidifier. Try a different mask. Talk to your doctor. CPAP isn’t perfect-but it’s the most effective treatment for sleep apnea we have. And if you stick with it, you’ll wonder how you ever slept without it.
Why do I wake up with a dry mouth even with a humidifier?
Dry mouth from CPAP is usually caused by mouth breathing, not low humidity. When you breathe through your mouth, the pressurized air escapes, drying out your throat. The solution isn’t turning up the humidifier-it’s stopping mouth breathing. Use a chin strap or switch to a full-face mask to keep air flowing through your nose.
How do I know if my CPAP mask is leaking?
You’ll hear a hissing sound, see red marks on your face, or notice high leak rates on your machine’s app. A leak over 24 L/min reduces therapy effectiveness. Try the airflow test: With the machine on, gently pull the mask away until you hear air escaping, then push it back until the noise stops. That’s your seal. Also check for worn-out cushions-they need replacing every 3 months.
Can I adjust my CPAP pressure myself?
Most machines let you adjust pressure by ±2 cm H₂O, but going beyond that voids your warranty and can be unsafe. If you feel the pressure is too high or too low, check your machine’s data (AHI and leak rates). If your AHI is above 5 after two weeks, contact your sleep doctor. They’ll use your data to safely adjust your pressure. Don’t guess-let your doctor decide.
Is a full-face mask better than a nasal mask?
It depends. If you breathe through your mouth during sleep, a full-face mask is usually the best choice-it covers both nose and mouth, preventing air leaks and dry mouth. If you breathe only through your nose, a nasal mask is lighter and less claustrophobic. Many users start with a nasal mask and switch to full-face if they develop dry mouth or leaks. Try both if you can.
How long does it take to get used to CPAP?
Most people need 2-4 weeks to adjust. The first few nights are often uncomfortable-mask pressure, noise, dryness. But 78% of users who stick with it for 14 days report major improvements. Focus on small wins: use it for 4 hours a night, even if not all night. Gradually increase time. Use a chin strap, heated tubing, and clean your gear daily. Your body will adapt.
What’s the best CPAP machine for leaks and dry mouth?
The ResMed AirSense 11 is the top choice. It has advanced leak detection (down to 12 L/min), a heated humidifier with ClimateControl, and an AutoSet algorithm that adjusts pressure smoothly. It also has the quietest operation at 25-27 dB. Philips DreamStation 2 is a close second, especially if you use the DreamMapper app for personalized tips. Avoid older or basic models without heated tubing or smart pressure features.
Does Medicare cover CPAP repairs and replacements?
Yes. Medicare covers 80% of the cost of CPAP machines and supplies like masks, tubing, and filters after you meet your deductible. Masks and cushions are replaced every 3 months, tubing every 6 months, and machines every 5 years under Medicare guidelines. You’ll need a prescription and proof of usage (4+ hours/night for 70% of nights over 30 days) to keep coverage.
Can CPAP cause sinus infections?
Not directly. But if you don’t clean your equipment, bacteria or mold can build up in the mask, tubing, or water chamber-and that can lead to sinus irritation or infection. Always rinse your gear daily with mild soap and water, and let it air dry. Use distilled water in the humidifier, not tap water. If you get frequent sinus issues, talk to your doctor about nasal saline rinses or a filter upgrade.


satya pradeep
November 18, 2025 AT 17:55Kelsey Robertson
November 20, 2025 AT 06:03Tarryne Rolle
November 21, 2025 AT 03:20Joseph Townsend
November 21, 2025 AT 19:27Kyle Swatt
November 22, 2025 AT 19:50Kiran Mandavkar
November 23, 2025 AT 19:50Shannon Hale
November 25, 2025 AT 10:51Elia DOnald Maluleke
November 26, 2025 AT 21:52Eric Healy
November 28, 2025 AT 09:03saurabh lamba
November 30, 2025 AT 00:42Deb McLachlin
December 1, 2025 AT 02:02Gordon Mcdonough
December 2, 2025 AT 20:30Holli Yancey
December 3, 2025 AT 06:59Jeremy Hernandez
December 4, 2025 AT 22:58