Most people drink coffee or tea without thinking twice. But if you're taking medication, that morning cup could be doing more than just waking you up-it could be making your drugs less effective, or even dangerous. Caffeine isn't just a stimulant. It's a powerful chemical that interacts with your body’s ability to process medications, and those interactions can be serious-even life-threatening.
How Caffeine Changes How Your Body Handles Medications
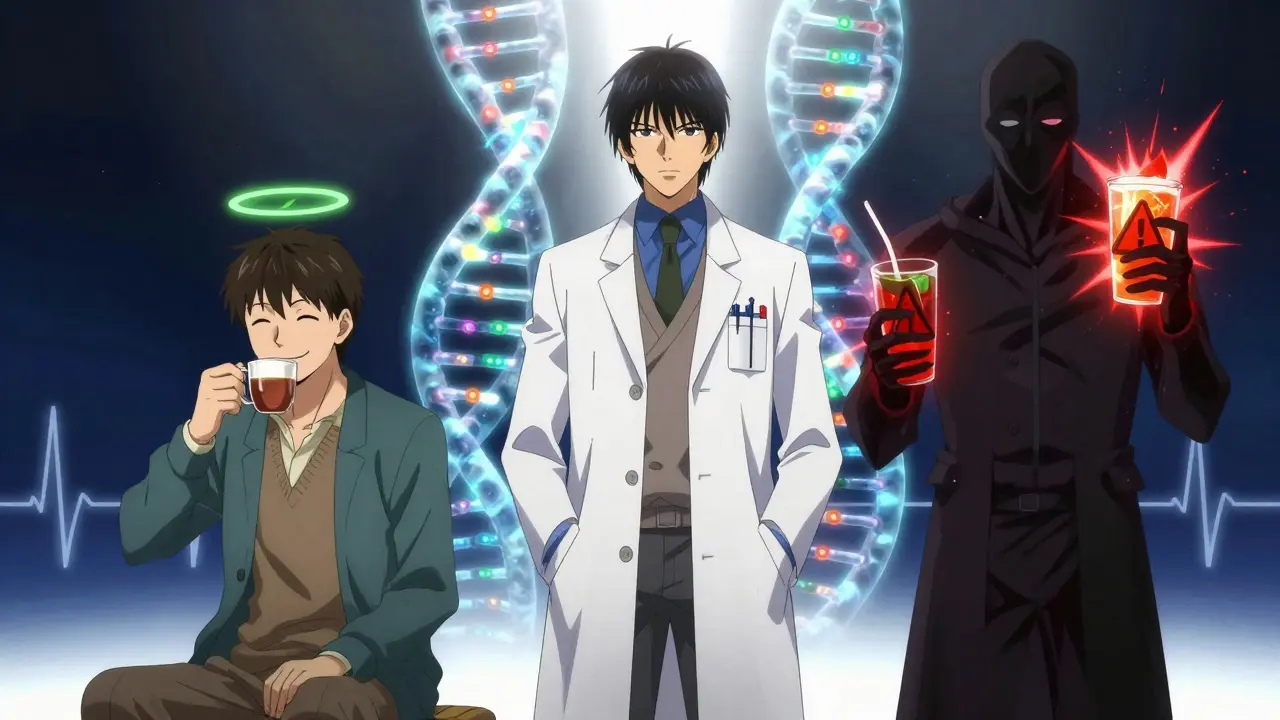
Caffeine doesn't just float around in your system. It actively interferes with enzymes in your liver that break down drugs. The main enzyme it messes with is called CYP1A2. This enzyme handles about 10% of all prescription medications. When caffeine blocks it, those drugs stick around longer than they should, or don’t get absorbed properly.
Think of it like traffic. Your liver is a busy intersection. Caffeine shows up and starts blocking the lanes where certain drugs are supposed to pass through. Some drugs get stuck. Others never even make it to their destination. The result? You might not feel the full effect of your medication, or you might get hit with too much of it all at once.
And it’s not just coffee. Energy drinks, soda, chocolate, and even some supplements contain caffeine. One energy drink can pack 80 to 300 mg of caffeine-more than a cup of coffee-and often includes other ingredients like taurine or ginseng that can make things worse.
High-Risk Medications: What to Watch Out For
Some medications have well-documented, dangerous interactions with caffeine. These aren’t rare edge cases. They’re common prescriptions that millions take every day.
Warfarin (Blood Thinners)
If you’re on warfarin to prevent clots, caffeine can raise your INR levels by 15-25% within 24 hours. That means your blood takes longer to clot, increasing your risk of bleeding-sometimes severely. One study found that 41% of warfarin patients who drank more than 200 mg of caffeine daily had unexplained INR spikes above 4.0. Some ended up in the ER with internal bleeding.
The FDA says you need to keep your caffeine intake consistent. Don’t suddenly switch from one cup a day to four. That spike can throw your dosing off. Even if you’ve been stable for months, a new energy drink habit can undo all that.
Levothyroxine (Thyroid Medication)
Many people take levothyroxine for hypothyroidism. But if you take it with coffee, your body absorbs up to 55% less of the drug. One patient reported their TSH level jumped from 1.8 to 8.7 after drinking coffee with their pill for three weeks. That’s a huge swing-enough to cause fatigue, weight gain, and even heart problems.
The American Thyroid Association says wait at least 60 minutes after taking your pill before drinking coffee. Some experts recommend waiting two hours. Don’t rely on feeling fine. Blood tests are the only way to know if your dose is still working.
Theophylline (Asthma Medication)
Theophylline and caffeine are chemically similar. They both use the same liver pathway. When you drink caffeine while taking theophylline, your blood levels of the drug can rise by 15-20%. That’s enough to cause nausea, rapid heartbeat, tremors, or even seizures-even at normal doses.
Patients on theophylline should limit caffeine to less than 100 mg per day (about one small coffee). And they should watch for heart rates over 100 bpm. That’s a red flag.
SSRIs (Antidepressants)
Fluvoxamine, an SSRI, has a known interaction with caffeine. Studies show caffeine can reduce its absorption by about 33%. That means your depression symptoms might not improve, even if you’re taking the right dose. Users on Reddit report increased anxiety, jitteriness, and insomnia when combining caffeine with SSRIs.
Not all antidepressants act the same. Bupropion doesn’t interact much with caffeine. But if you’re on fluoxetine, sertraline, or fluvoxamine, treat caffeine like a drug you’re not supposed to mix.
Cardiovascular Drugs: Adenosine, Dipyridamole, Verapamil
Adenosine and dipyridamole are used in cardiac stress tests. If you’ve had coffee, tea, or soda in the past 24 hours, those tests can fail. Caffeine blocks their effect by 70-90%. You might need to reschedule your test-and delay important heart diagnostics.
Verapamil, a blood pressure medication, loses 25-30% of its effectiveness when taken with coffee. Harvard Health found that patients who drank coffee within two hours of their dose had significantly higher blood pressure readings. The fix? Take your coffee at least two hours before or after your pill.
Pseudoephedrine and Ephedrine (Cold and Allergy Meds)
Decongestants like pseudoephedrine already raise heart rate and blood pressure. Add caffeine, and you get a double hit. One cardiologist described it as a “one-two punch.” Heart rates can jump 20-30 beats per minute in sensitive people. In clinical trials, combining ephedrine with caffeine raised systolic blood pressure by over 30 mmHg in 68% of cases-and increased the risk of hypertensive crisis by 47%.
These aren’t theoretical risks. Real people have ended up in emergency rooms after taking cold medicine and drinking coffee.

Who’s at Greatest Risk?
Not everyone reacts the same. Genetics play a big role. Some people have a version of the CYP1A2 gene that breaks down caffeine slowly. For them, caffeine stays in the system for up to 9.5 hours-or even longer if they have liver disease. In newborns, it can last nearly four days.
People on multiple medications are especially vulnerable. A 2021 study found that patients taking five or more daily drugs were 3.2 times more likely to have a clinically significant caffeine interaction. That includes diabetics, heart patients, and older adults on complex regimens.
Energy drinks are a growing concern. They’re not just caffeine-they’re caffeine plus sugar, taurine, guarana, and other stimulants. Between 2020 and 2024, the FDA saw a 37% jump in adverse event reports tied to caffeine-medication interactions, and 68% of serious cases involved energy drinks.
What Should You Do?
You don’t need to quit caffeine entirely. But you do need to be smart about it.
- Know your meds. Check the label. If it says “avoid caffeine” or “may interact with stimulants,” take it seriously.
- Time it right. Wait at least 60 minutes after taking levothyroxine. Wait two hours before or after verapamil. Avoid caffeine for 24 hours before cardiac stress tests.
- Track your intake. Write down how much caffeine you have each day. A cup of coffee = 95-200 mg. A can of soda = 30-40 mg. An energy drink = 80-300 mg.
- Don’t change habits suddenly. If you drink coffee every day, keep doing it. If you don’t, don’t start. Sudden changes can destabilize your medication levels.
- Talk to your pharmacist. They’re trained to catch these interactions. Ask them: “Does my medication interact with caffeine?”
What’s Changing in 2025?
Healthcare is catching up. In 2023, the American Pharmacists Association made caffeine interaction screening mandatory for certified pharmacists. Now, they’re required to check for 17 high-risk combinations during medication reviews.
Pharmaceutical companies are updating labels. Twenty-three percent of prescription drugs now include caffeine interaction warnings-up from 12% in 2019.
And technology is helping. Epic Systems rolled out a pilot program in 47 hospitals in April 2025 that flags potential caffeine-medication conflicts in electronic records. Early results show a 29% drop in related adverse events.
By 2028, experts predict personalized caffeine guidance based on genetic testing will become standard. If you have a slow-metabolizer gene, your doctor might tell you to cut caffeine completely. If you’re a fast metabolizer, you might be able to have your coffee safely.
Bottom Line: Don’t Assume It’s Safe
Most people don’t realize caffeine is a drug interaction risk. A 2024 JAMA study found 62% of patients had no idea their coffee could interfere with their meds-even though 89% drank it daily.
If you take any prescription or over-the-counter medication, assume caffeine could affect it until you prove otherwise. Talk to your doctor or pharmacist. Don’t wait for a bad reaction. Don’t rely on internet forums or anecdotal advice. Use the data. Use the guidelines. Use your brain.
That cup of coffee might seem harmless. But when it’s mixed with the wrong medication, it’s not just a morning ritual-it’s a health risk.


Melissa Taylor
December 15, 2025 AT 17:58Thank you for this. I’ve been on warfarin for years and never realized my afternoon espresso could be throwing off my INR. I’ve switched to decaf after 2pm and my numbers have stabilized. Small changes matter.
John Brown
December 17, 2025 AT 00:33I used to chug energy drinks before my cardio workouts. Then I got put on verapamil. My BP spiked so hard I thought I was having a stroke. Now I just drink water. No regrets. Your body isn’t a lab experiment.
Christina Bischof
December 18, 2025 AT 08:49My mom takes levothyroxine and coffee. She swears she’s fine. Her TSH was 9.2 last check. She still doesn’t believe it’s the coffee. Sometimes people just don’t want to change.
Jocelyn Lachapelle
December 20, 2025 AT 02:48I didn’t know caffeine could mess with SSRIs. I’ve been on sertraline for two years and I drink three cups a day. No wonder I’ve been so jittery lately. Going to cut back and see what happens. Thanks for the wake-up call.
Mike Nordby
December 20, 2025 AT 04:49The CYP1A2 enzyme polymorphism data cited here is robust. The pharmacokinetic interference is well-documented in clinical pharmacology literature, particularly in the Journal of Clinical Pharmacology, 2022. Consistency in intake is paramount for therapeutic drug monitoring. Further, the FDA’s guidance on caffeine variability in anticoagulant therapy is underappreciated by primary care providers.
Sai Nguyen
December 20, 2025 AT 17:25Americans think caffeine is harmless. In India, we know stimulants are drugs. You people drink coffee like water and wonder why you’re sick.
Nupur Vimal
December 21, 2025 AT 23:59Everyone’s so scared of caffeine but nobody talks about how sugar in energy drinks is worse. You’re all ignoring the real problem. Sugar kills. Not caffeine.
Cassie Henriques
December 22, 2025 AT 21:23Big pharma’s pushing this narrative because they want you to buy their ‘caffeine-free’ versions. CYP1A2 inhibition is dose-dependent. One cup? Fine. Three? Maybe not. But don’t let them scare you into buying overpriced decaf.
Benjamin Glover
December 23, 2025 AT 07:20Typical American overreaction. In the UK, we’ve known this since the 80s. You don’t need a 2000-word article to tell you not to mix caffeine with warfarin. Basic pharmacology.
Raj Kumar
December 24, 2025 AT 15:26bro i take theo and coffee and never had a prob but maybe im just lucky. also my auntie says she takes thyroid med with tea and shes fine. maybe its just me?
John Samuel
December 24, 2025 AT 21:58This is a masterclass in patient-centered pharmacovigilance. The integration of genetic predisposition, real-world behavioral patterns, and technological intervention represents a paradigm shift in clinical safety protocols. Kudos to Epic Systems for pioneering this in EHRs. This is the future of personalized medicine.
Michelle M
December 25, 2025 AT 11:16It’s funny how we treat caffeine like a harmless ritual while ignoring how deeply it’s woven into our culture’s idea of productivity. Maybe the real issue isn’t the interaction-it’s that we’ve normalized pushing our bodies beyond their limits just to keep up.
Lisa Davies
December 25, 2025 AT 18:42Just started taking levothyroxine last month. I switched to drinking coffee 90 mins after my pill. I feel like a new person. ☕️💙