Buprenorphine Dose Effect Calculator
How Buprenorphine Works
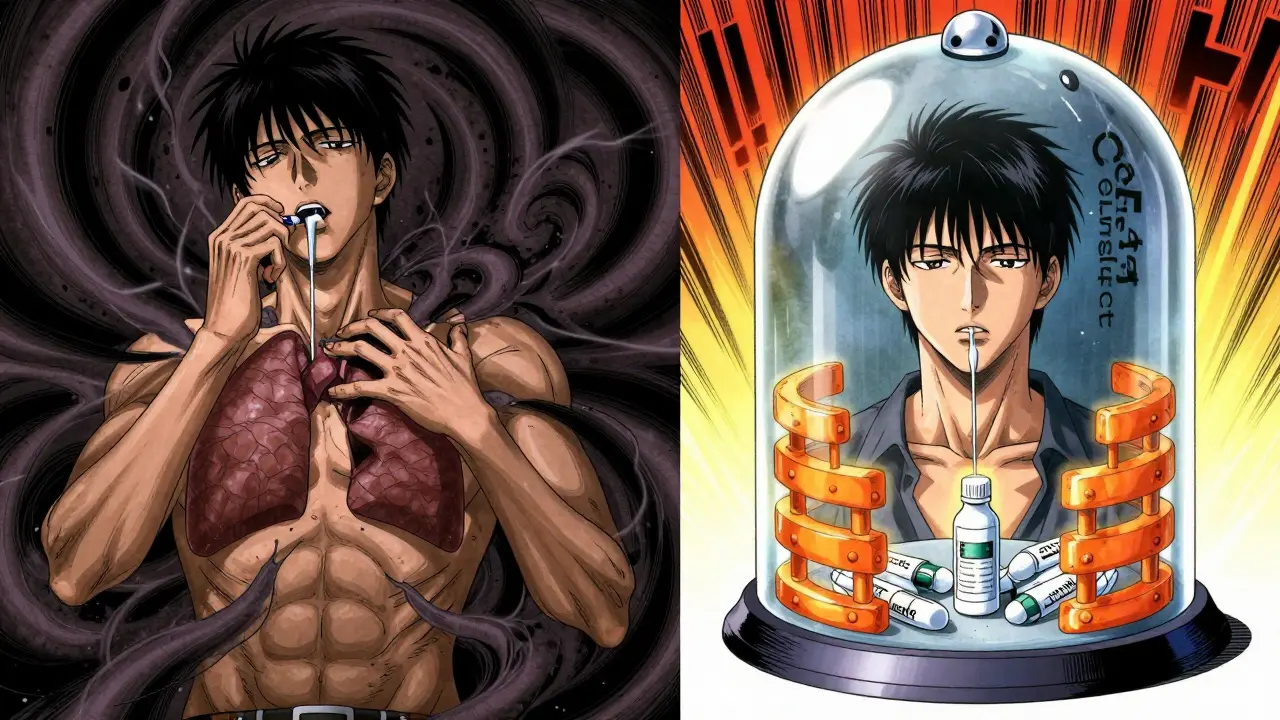
This tool demonstrates the ceiling effect of buprenorphine—how it stabilizes at a specific dose without increasing respiratory depression risk.
Results
Adjust the dose slider to see how buprenorphine's effects change.
When someone is trying to get off opioids, the biggest fear isn’t withdrawal-it’s dying from an overdose. That’s why buprenorphine changed everything. Unlike heroin, oxycodone, or even methadone, buprenorphine has a built-in safety feature called the ceiling effect. This isn’t just a pharmacology term. For people in recovery, it means they can take enough to stop cravings and stay off other drugs without risking their breathing. And that’s why millions now choose it over older treatments.
What Is the Ceiling Effect, Really?
The ceiling effect isn’t magic. It’s science. Buprenorphine binds tightly to opioid receptors in the brain, but it doesn’t fully turn them on. Think of it like a dimmer switch instead of an on/off button. At low doses, it gives you relief. At higher doses, it stops getting stronger-especially when it comes to slowing your breathing.
Research shows that after about 24 mg per day, increasing the dose doesn’t make respiratory depression worse. That’s the ceiling. Even if someone takes 70 mg, their breathing doesn’t slow down any further than it would at 24 mg. That’s not true for full agonists like heroin or oxycodone. With those, more dose = more danger. With buprenorphine, more dose = more stability.
This is why overdose deaths from buprenorphine alone are rare. The U.S. Centers for Disease Control and Prevention (CDC) found that between 2019 and 2021, only 18 fatal overdoses involved buprenorphine-and every single one also included benzodiazepines, alcohol, or other depressants. Alone, buprenorphine doesn’t kill. Combined with other drugs, it can. But the ceiling still holds. It doesn’t make you invincible. It just gives you a huge buffer.
Why Buprenorphine Is Safer Than Methadone
Methadone has been used for decades to treat opioid use disorder. But it’s a full opioid agonist. That means it can produce strong euphoria and, more importantly, it can shut down breathing at high doses. People on methadone need to go to a clinic every day. They’re monitored. Why? Because the risk is real.
Buprenorphine doesn’t need that. It’s safe enough to prescribe in a doctor’s office. In 2022, about half of all medication-assisted treatment prescriptions in the U.S. were for buprenorphine. Only 35% were for methadone. That shift didn’t happen by accident. It happened because patients and doctors saw the difference.
One study showed that patients on 16 mg of buprenorphine had the same level of opioid blockade against heroin as those on 8 mg-but no extra high. With methadone, doubling the dose doubles the euphoria. With buprenorphine, it doesn’t. That’s why people say they can work, drive, and parent while on it. They’re not drugged. They’re stabilized.
Common Side Effects-And How They Compare
No drug is side effect free. Buprenorphine is no exception. But compared to full agonists, its side effects are mild and manageable.
- Headache: Happens in about 18% of people during the first few weeks. Usually fades. Over-the-counter painkillers help.
- Constipation: Affects 12% of users. Less severe than with oxycodone or hydrocodone. Drinking water and eating fiber helps.
- Nausea: About 10% report it. Often goes away after a few days.
- Precipitated withdrawal: This isn’t a side effect of the drug itself-it’s a mistake in timing. If you take buprenorphine too soon after your last opioid, it can kick out the other drugs from your receptors and cause sudden, intense withdrawal. That’s why doctors wait 12-24 hours after last use before starting. About 25% of people who start too early experience this. It’s avoidable.
- Sedation: Rare at standard doses. Unlike methadone, which can make people feel foggy all day, buprenorphine usually doesn’t cause drowsiness unless mixed with alcohol or benzodiazepines.
Patients in recovery often say the biggest win isn’t the lack of euphoria-it’s the lack of fatigue. One Reddit user wrote: “I take my 16mg and go to work without feeling like I’m on something, which methadone never allowed.” That’s the ceiling effect in action.
Who Needs Higher Doses?
Not everyone responds the same. Some people with long-term, severe opioid dependence need more than 16 mg to feel stable. Clinical guidelines say 8-16 mg is typical, but up to 24 mg is the safe upper limit. Some patients, especially those with chronic pain or heavy prior opioid use, may need doses at the higher end.
A 2023 study from the MCSTAP network found that patients with chronic pain needed higher buprenorphine doses to control cravings-but still stayed under the respiratory ceiling. That’s important. It means the safety profile holds even when the dose goes up. The ceiling isn’t a limit on effectiveness. It’s a limit on danger.
Doctors don’t just guess the right dose. They start low-2-4 mg-and slowly increase every few hours on the first day, watching for signs of withdrawal or sedation. Most patients stabilize within a week. The goal isn’t to get high. It’s to feel normal.
The Blockade Effect: How It Stops Relapse
Buprenorphine doesn’t just treat cravings. It blocks other opioids. Because it binds so tightly to receptors, if someone takes heroin or oxycodone while on buprenorphine, those drugs can’t attach. It’s like a locked door. Even if you have the key, the lock won’t turn.
At 16 mg, buprenorphine blocks about 90% of heroin’s effects. At 8 mg, it’s closer to 70%. That’s why higher doses are more effective for people with high tolerance. It’s not about feeling more. It’s about feeling nothing else.
This blockade effect lasts a long time. Buprenorphine sticks to receptors for 6-8 hours before it starts to leave. That’s why many people can take it once a day-or even every other day. Some newer formulations, like the monthly Sublocade injection, keep levels steady for weeks. No daily pills. No missed doses. Just steady protection.

What About Overdose Risk?
Yes, you can overdose on buprenorphine. But it’s not common. And it’s almost always when it’s mixed with other depressants. Benzodiazepines (like Xanax or Valium), alcohol, or sleeping pills are the real killers. Together, they can overwhelm the brain’s breathing center-even with buprenorphine’s ceiling.
That’s why doctors always ask: “Are you taking anything else?” If you are, they’ll adjust. Or they’ll help you taper off the other drugs first. The ceiling protects you from buprenorphine alone. It doesn’t protect you from combinations.
Also, don’t assume that because it’s safer, you can skip medical supervision. Starting buprenorphine without a doctor’s guidance is dangerous. You need the right timing, the right dose, and monitoring for withdrawal or interactions.
New Forms, Same Safety
In 2023, the FDA approved Sublocade-a monthly injection of buprenorphine. It’s a game-changer for people who struggle with daily pills. Clinical trials showed 49% of patients stayed abstinent for 26 weeks, compared to 35% on daily sublingual tablets. And the ceiling effect? Still there. No extra risk. Just better adherence.
Other new formulations are in development, including extended-release implants and prodrug combinations designed to improve absorption without losing safety. The goal isn’t to make it stronger. It’s to make it easier to use-while keeping the ceiling intact.
Final Thoughts: It’s Not Perfect, But It’s Life-Saving
Buprenorphine isn’t a cure. It’s a tool. It works best when paired with counseling, peer support, and a plan for long-term recovery. But even without those, it saves lives. It reduces overdose deaths. It keeps people out of jail. It lets them hold jobs and care for their kids.
The ceiling effect is what makes it different. It’s not just a chemical quirk. It’s a public health breakthrough. For people who’ve lost everything to opioids, it offers something rare: safety with stability. You don’t have to feel high to get well. And you don’t have to risk dying to stay off drugs.
If you’re considering buprenorphine, talk to a provider who knows how to use it. Don’t let fear of side effects stop you. The real danger isn’t buprenorphine. It’s staying stuck in the cycle of withdrawal, craving, and overdose.


Priya Patel
January 12, 2026 AT 09:43Buprenorphine saved my life. I was on heroin for 8 years. Tried methadone, felt like a zombie. Started buprenorphine at 8mg, now at 16mg, and I’m working, hiking, even dating again. No fog. No crash. Just steady. The ceiling effect isn’t just science-it’s freedom.
Alfred Schmidt
January 13, 2026 AT 03:45Stop glorifying this drug. People die from buprenorphine every day-especially when they mix it with Xanax. You think the ceiling protects you? It’s a lie. The CDC data is cherry-picked. What about the people who overdose on buprenorphine and then get buried in the ‘other drugs’ category? It’s all connected. Stop pretending it’s safe.
Priscilla Kraft
January 14, 2026 AT 15:05Hey, I get where you're coming from, but the data doesn't lie. Buprenorphine alone is incredibly safe. I'm a nurse in an addiction clinic, and I've seen hundreds of patients transition from methadone to buprenorphine. The difference in their energy, mood, and ability to function is night and day. Yes, mixing with benzos is dangerous-but that's true for ANY opioid. The point is, buprenorphine gives people a fighting chance. 🙏
Michael Patterson
January 14, 2026 AT 17:37Look, I’ve been in recovery for 11 years, and I’ve tried everything. Methadone made me feel like I was underwater. Buprenorphine? I took 4mg on day one, and by day three I was back at work, no grogginess, no cravings, no guilt. The ceiling effect? It’s real. I’ve taken 30mg just to see what happens-nothing. My breathing didn’t slow. My head didn’t spin. I just felt… normal. That’s the miracle. Not euphoria. Normalcy. That’s what we were all fighting for.
Matthew Miller
January 15, 2026 AT 13:09Everyone’s acting like buprenorphine is a miracle drug. It’s not. It’s just another opioid. You’re just replacing one addiction with another. You think you’re ‘stable’? You’re still chemically dependent. And don’t even get me started on the pharma companies pushing this stuff because it’s profitable. You’re not free-you’re just on a different leash.
Vincent Clarizio
January 17, 2026 AT 12:12Let’s be real: the ceiling effect is a marketing term dressed up as science. The real reason buprenorphine is safer is because it’s a partial agonist with low intrinsic activity. But let’s not pretend it’s harmless. People still get addicted. People still abuse it. And yes, even at 24mg, if you’re a heroin addict with zero tolerance, you can still OD if you’re dumb enough to stack it with alcohol and Klonopin. The ceiling isn’t a force field-it’s a suggestion. And some people ignore suggestions. Especially the ones who think they’re invincible.
Adewumi Gbotemi
January 17, 2026 AT 17:27I’m from Nigeria. We don’t have much access to this medicine. But I read about it online. My cousin died from overdose. If this drug can help people live without dying, then it’s good. Simple. No need to overthink. Just help people.
Jason Shriner
January 17, 2026 AT 23:56So… we’re giving people a drug that makes them feel ‘normal’… so they can go back to their 9-to-5 and pretend life isn’t a dumpster fire? Cute. The ceiling effect is just capitalism’s way of keeping addicts functional enough to pay rent but not so high they can enjoy life. Brilliant. We’ve turned recovery into a productivity hack.
Sean Feng
January 18, 2026 AT 19:43Why are we even talking about this? Just let people use whatever they want. If they OD, they OD. The state shouldn’t be playing doctor.
Madhav Malhotra
January 18, 2026 AT 23:05In India, we don’t have access to buprenorphine easily. But I’ve seen people on methadone-drowsy all day, can’t work, can’t care for kids. If this drug lets someone be present in their life again? That’s worth more than any side effect list. I’m not a doctor, but I know what presence looks like. And this gives it back.
Sam Davies
January 20, 2026 AT 12:57Oh, so now we’re romanticizing pharmacological moderation? How quaint. Next you’ll tell me the ceiling effect is the reason we finally stopped treating addicts like criminals. Newsflash: it’s not. It’s because the opioid crisis made the CDC panic and the DEA finally ran out of excuses. Buprenorphine didn’t save lives-it just made the paperwork prettier.
Alex Smith
January 21, 2026 AT 02:38So… if someone takes 70mg of buprenorphine and doesn’t die, does that mean they’re ‘safe’? Or does it mean they’re just lucky? The ceiling isn’t a guarantee-it’s a probability curve. And probability doesn’t care if you’re a parent, a veteran, or a college student. It just is. So maybe stop calling it a miracle and start calling it what it is: a tool with limits. And tools need hands. And hands need guidance.
Jennifer Littler
January 21, 2026 AT 22:27Just wanted to add: the 2023 MCSTAP study on chronic pain patients using higher doses? That’s the real story. The ceiling holds even when the dose climbs. That’s not luck. That’s design. And for people who’ve been told for years that their pain is ‘all in their head,’ being able to stabilize without risking respiratory failure? That’s not just clinical-it’s human.