Most people think hearing aids go in the ear. But what if the solution doesn’t need to go in the ear at all? Bone-conduction hearing aids work by sending sound straight through your skull bone to the inner ear, skipping the outer and middle ear entirely. This isn’t science fiction-it’s a proven, FDA-approved option for people who can’t use traditional hearing aids because of chronic ear infections, birth defects, or single-sided deafness.
How Bone-Conduction Hearing Aids Actually Work
Sound normally travels through the air, into your ear canal, vibrates your eardrum, and moves tiny bones in your middle ear before reaching the cochlea. But if your ear canal is blocked, your eardrum is damaged, or your middle ear bones don’t move right, that path is broken. Bone-conduction devices bypass all of that. They use vibrations-like tapping your finger on your temple-to send sound directly to the cochlea through the bone of your skull.
This isn’t new. The science behind it goes back to the 1950s, when Swedish surgeon Per-Ingvar Brånemark discovered titanium could fuse with bone. That breakthrough led to the first bone-anchored hearing aid in 1977. Today, devices like Cochlear’s BAHA, Oticon’s Ponto, and MED-EL’s Bonebridge use the same principle. They don’t rely on air. They rely on bone.
The key difference between these and regular hearing aids? No ear molds. No wax buildup. No blocked ear canals. If you’ve had recurring ear infections or were born with a malformed ear canal, this is often the only way to get clear sound without constant irritation or risk of infection.
Who Benefits Most from Bone-Conduction Devices
These aren’t for everyone. They’re designed for three main groups:
- Conductive hearing loss: When sound can’t travel through the outer or middle ear. This includes people with chronic ear infections, earwax blockages that won’t clear, or congenital conditions like aural atresia (a missing or closed ear canal).
- Mixed hearing loss: A combination of conductive and sensorineural loss. If your inner ear is partially damaged but your outer/middle ear is the bigger problem, bone conduction can still help.
- Single-sided deafness (SSD): When one ear is completely deaf and the other works fine. Traditional hearing aids can’t help here. Bone-conduction devices pick up sound from the deaf side and send it to the good ear, letting you hear people on your bad side and locate where sounds come from.
Studies show these devices improve speech understanding in noisy environments by 20-35% for SSD patients. For people with aural atresia, success rates are 85-90%. In contrast, regular hearing aids often don’t work at all for these cases-up to 92% of chronic ear infection patients are medically disqualified from using them.
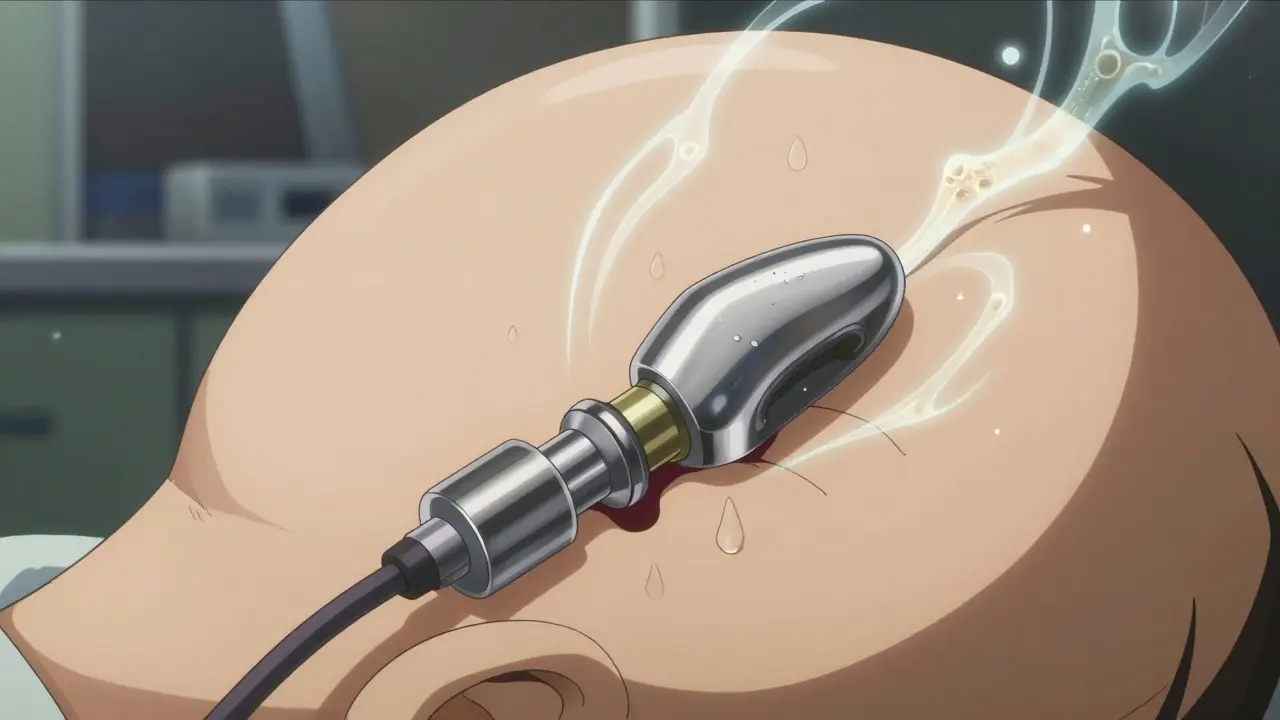
Percutaneous vs. Transcutaneous: Two Different Systems
There are two main types of bone-conduction devices: those that go through the skin and those that don’t.
Percutaneous systems (like Cochlear BAHA Connect and Oticon Ponto 5) require a titanium implant fused to the skull bone. After surgery, a small metal post sticks out through the skin. The sound processor snaps onto it. These are powerful-up to 50 dB of gain-and give the clearest signal. But they come with a trade-off: skin problems. About 15-30% of users develop redness, irritation, or infection around the abutment. Daily cleaning with 70% isopropyl alcohol is required. About 8% need revision surgery.
Transcutaneous systems (like MED-EL Bonebridge and Cochlear BAHA Attract) use magnets. The implant sits under the skin, and the external processor holds on via magnetic force. No hole in the skin means no infection risk. The downside? The skin and tissue between the processor and bone weaken the signal by 10-15 dB. That’s fine for mild to moderate loss, but not enough for severe cases. These are also invisible under hair, which many users prefer.
As of 2023, 63% of new bone-conduction implants are transcutaneous-up from 41% in 2019. People are choosing them for comfort, not just appearance.
Cost, Surgery, and Recovery
Getting a bone-conduction device isn’t like walking into a hearing clinic and walking out with a hearing aid. It requires minor surgery.
The procedure takes 30-60 minutes under local anesthesia. Most people go home the same day. Recovery is quick-normal activities resume in 48 hours. But the device doesn’t start working right away.
For percutaneous systems, the titanium implant needs 3-4 months to fuse with the bone before the processor can be attached. Transcutaneous systems can be activated immediately after surgery. But even then, your brain needs time to adjust. It takes 2-4 weeks to get used to hearing sound through your skull. Audiologists recommend auditory training-listening exercises-to help your brain interpret the new signals.
Cost is a big factor. Implantable bone-conduction devices range from $4,000 to $7,000 per ear. Premium air-conduction hearing aids cost $1,500-$3,500. Insurance often covers bone-conduction devices if you have a documented medical reason (like chronic infection or congenital malformation). Medicare and many private insurers recognize them as medically necessary, not cosmetic.
Real People, Real Results
Reddit users with single-sided deafness describe life-changing results. One person wrote: "I heard birds chirping from my deaf side for the first time in 15 years." Another said they could finally hear their child calling from behind them at the park.
On hearing forums, 78% of recent posts from SSD users report major improvements. People love the natural sound quality and the fact that their ears stay completely open. No more itching. No more muffled voices. No more feeling like they’re wearing a plug.
But it’s not perfect. About 23% of users complain about MRI scans. Most implants are made of titanium, which is safe, but the external processor and magnets can interfere with 1.5T or higher machines. Some people have to have the implant removed before an MRI-something no one wants to hear.
And while transcutaneous systems avoid skin issues, they’re not for everyone. If your hearing loss is severe (over 55 dB), the signal loss through skin makes them ineffective. That’s why doctors still recommend percutaneous systems for people with the worst conductive loss.

The Future: Fully Implantable and Smarter
Technology is moving fast. Cochlear’s BAHA 6 Max, released in 2023, has Bluetooth 5.3, direct streaming to smartphones, and a 30-hour battery. MED-EL’s Bonebridge 3, coming in 2024, uses AI to adjust sound in real time based on your environment.
The biggest leap? Fully implantable systems. No external processor at all. Sonova is already in Phase III trials for one. If approved, it could be on the market by late 2024. Imagine a device you never see, never touch, never charge. Just hear.
Market growth is strong. Bone-conduction devices make up just 5.2% of the global hearing aid market today, but they’re growing at 8.7% per year-more than double the rate of traditional aids. Scandinavia leads adoption, with 1.2% of hearing-impaired Swedes using them. In the U.S., it’s only 0.4%. But awareness is rising. Nine million Americans have single-sided deafness-and only 15% are treated. That’s a huge untapped need.
When Bone-Conduction Isn’t the Right Choice
These devices don’t help if your cochlea is severely damaged. If your inner ear can’t process sound, vibrating the bone won’t fix it. They’re not for age-related sensorineural hearing loss unless there’s also a conductive component.
They’re also not ideal for people who can’t commit to surgery or follow-up care. Daily cleaning, regular check-ups, and understanding the limitations (like MRI issues) are part of the package.
If you’re young, active, and have a mild hearing loss, a regular hearing aid or even a CROS system might be simpler and cheaper. But if you’ve been told you can’t use traditional aids-or if you’ve tried them and they just don’t work-bone conduction might be the answer you’ve been waiting for.
Can bone-conduction hearing aids restore normal hearing?
No, they don’t restore normal hearing. They bypass damaged parts of the ear to deliver sound directly to the cochlea. For people with conductive or mixed hearing loss, they can provide clear, natural sound. For single-sided deafness, they restore spatial awareness and help hear from both sides. But they can’t fix damage to the inner ear itself.
Do bone-conduction devices work for children?
Yes. Children as young as five can get bone-conduction implants, especially those born with aural atresia or chronic ear infections. Softband versions (non-surgical headbands with processors) are available for younger kids, letting them try the technology before committing to surgery. Success rates in children are high-85-90%-and early use supports language development.
Are bone-conduction hearing aids covered by insurance?
Often, yes-if you have a documented medical need. Medicare, Medicaid, and most private insurers cover them for conductive or mixed hearing loss, single-sided deafness, or congenital ear malformations. They’re classified as medically necessary, not elective. You’ll need a diagnosis from an audiologist and a letter of medical necessity from your ENT.
Can I swim or shower with a bone-conduction hearing aid?
You can swim and shower with transcutaneous systems like Bonebridge or BAHA Attract-they’re waterproof when the processor is attached. Percutaneous systems require the external processor to be removed before water exposure. Most processors are water-resistant, not waterproof, so avoid submerging them. Always check manufacturer guidelines.
How long do bone-conduction devices last?
The titanium implant is designed to last a lifetime. The external processor typically lasts 5-7 years before needing replacement due to battery wear, technology upgrades, or damage. Some users upgrade sooner for better features like Bluetooth or noise reduction. The internal magnet in transcutaneous systems is also long-lasting and rarely needs replacement.
What’s the biggest downside of bone-conduction hearing aids?
The biggest downside is the surgery and potential complications. Skin issues around percutaneous abutments affect up to 30% of users, and some require revision surgery. MRI compatibility is another issue-though titanium implants are safe, the external parts can interfere with scans. Cost is also higher than traditional aids, and not everyone qualifies.


Dusty Weeks
January 2, 2026 AT 01:29Sally Denham-Vaughan
January 2, 2026 AT 08:57Bill Medley
January 3, 2026 AT 22:54Ann Romine
January 4, 2026 AT 10:26Austin Mac-Anabraba
January 5, 2026 AT 17:45Phoebe McKenzie
January 5, 2026 AT 18:05gerard najera
January 6, 2026 AT 08:38Stephen Gikuma
January 7, 2026 AT 06:06Bobby Collins
January 8, 2026 AT 01:52