Take your antibiotic with your antacid. Sounds simple, right? But if you do that, your antibiotic might not work at all. This isn’t a myth. It’s a well-documented, common, and preventable mistake that leads to treatment failure - especially with antibiotics like ciprofloxacin or doxycycline. If you’re on antibiotics and also take antacids for heartburn or indigestion, the timing between doses isn’t just a suggestion. It’s the difference between getting better and staying sick.
Why Antacids Mess With Antibiotics
Antacids like Tums, Rolaids, Maalox, or Mylanta contain minerals like aluminum, magnesium, or calcium. These minerals don’t just neutralize stomach acid - they also bind tightly to certain antibiotics. This binding creates a chemical cage around the drug, trapping it in your gut so your body can’t absorb it. The result? The antibiotic never reaches the infection in enough strength to kill the bacteria.It’s not just about stomach pH. While raising stomach acidity does affect how some drugs dissolve, the real culprit is chelation. That’s the scientific term for when metal ions in antacids latch onto antibiotic molecules. For example, ciprofloxacin (a fluoroquinolone) can lose up to 90% of its absorption when taken with an antacid containing aluminum or magnesium. That’s not a small drop - that’s nearly the whole dose wasted.
Even doxycycline, often thought of as more forgiving, still sees about 30% less absorption when paired with antacids. And tetracycline? It’s one of the most sensitive. A single antacid tablet can cut its effectiveness in half.
Which Antibiotics Are Most at Risk?
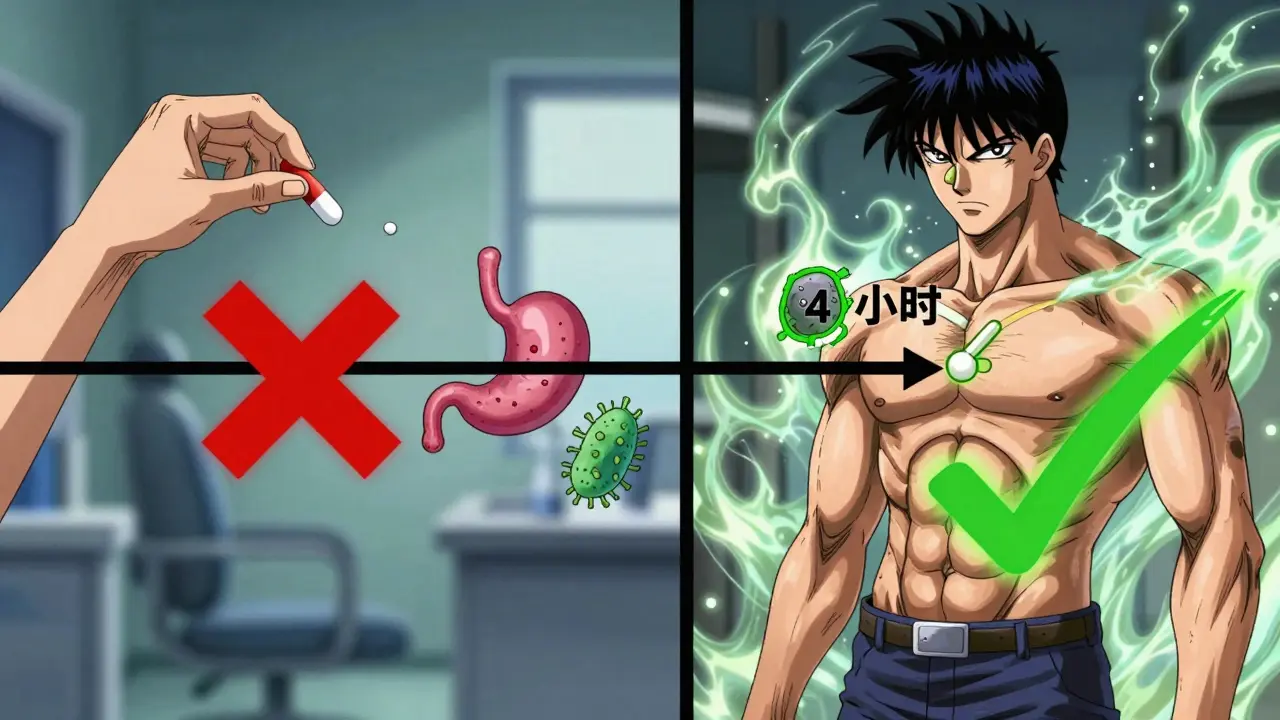
Not all antibiotics are affected the same way. Some are barely touched by antacids. Others? They’re highly vulnerable.- Fluoroquinolones - ciprofloxacin, levofloxacin, moxifloxacin: These are the most sensitive. Absorption drops by 75-90%. You need at least 2 hours before or 4 hours after an antacid.
- Tetracyclines - doxycycline, tetracycline: These are next in line. Absorption drops 50-70%. Separate doses by 2-3 hours.
- Penicillins and cephalosporins - amoxicillin, cephalexin: These are mostly safe. You might lose 15-20% absorption, but it rarely causes treatment failure. Still, 1-2 hours apart is smart.
- Macrolides - azithromycin, clarithromycin: Minimal interaction. Still, 2 hours separation is recommended as a safety buffer.
- Metronidazole: No significant interaction. You can take it with antacids without worry.
Here’s the key takeaway: if your antibiotic is on the first two lists, timing matters. A lot.
Real Consequences of Getting It Wrong
This isn’t just theoretical. People are getting sicker because they don’t know this.One study of 15,000 patients found that those who took ciprofloxacin with antacids had a 22% higher chance of their urinary tract infection coming back. Another report from a primary care clinic showed that 18% of apparent antibiotic failures were due to improper timing with antacids - not resistance, not wrong diagnosis, just bad timing.
On Reddit, a doctor shared that five patients in one year had recurring UTIs. All of them were taking Tums with their ciprofloxacin. Once they spaced the doses out by four hours, every single infection cleared up. No new prescriptions. No stronger drugs. Just better timing.
Patients on Amazon Pharmacy and Drugs.com report the same pattern: treatment fails. They go back to the doctor. They’re told they’re resistant. They get another antibiotic. It fails again. Then, a pharmacist asks, “Do you take antacids with your pills?” That’s when everything changes.
How to Space Them Out - Simple Rules
You don’t need a PhD to get this right. Here’s how to do it:- For ciprofloxacin, levofloxacin, or moxifloxacin: Take the antibiotic at least 4 hours before or 2 hours after your antacid. If you take your antibiotic at 8 a.m., wait until 12 p.m. or later for your antacid. If you take your antacid at 10 a.m., don’t take the antibiotic until 12 p.m.
- For doxycycline or tetracycline: Wait 2-3 hours between doses. Same logic: antibiotic first, then antacid - or vice versa, with enough space.
- For amoxicillin or cephalexin: 1-2 hours apart is enough. If you’re unsure, just wait 2 hours.
- For metronidazole: No timing needed. Take with or without antacids - your choice.
Pro tip: If you take your antibiotic twice a day - say, 8 a.m. and 8 p.m. - and you need antacids three times a day (after meals), plan your schedule around the antibiotic. Take antacids at 12 p.m. and 4 p.m. That gives you a 4-hour buffer before and after your antibiotic doses.
What If You Can’t Avoid Antacids?
Some people need daily acid control - GERD, ulcers, chronic heartburn. Stopping antacids isn’t an option. So what do you do?Switch to something that doesn’t interfere. H2 blockers like famotidine (Pepcid) or proton pump inhibitors like omeprazole (Prilosec) don’t contain aluminum, magnesium, or calcium. They work differently and rarely affect antibiotic absorption. A 2023 study showed that switching from antacids to omeprazole dropped treatment failure rates from 27% to just 9% in patients on antibiotics.
And if you’re on a long course of antibiotics? Ask your doctor if you can switch to a different antibiotic altogether. Metronidazole, for example, works great for many infections and doesn’t interact with antacids. Or consider newer formulations like Cipro XR-24 - a modified version of ciprofloxacin that only loses 8% absorption with antacids, compared to 90% for the regular version.

Tools to Help You Remember
Remembering to wait 2 or 4 hours between pills is harder than it sounds - especially if you’re juggling multiple meds, have a busy schedule, or are older.Use a pill organizer with time slots. Write it down on your calendar. Set alarms on your phone. But the best tool? Medication apps like MyMedSchedule. It’s used by over 1.2 million people and has built-in alerts for antacid-antibiotic interactions. When you log your antibiotic, it asks: “Are you taking an antacid?” If yes, it blocks the time window and reminds you when it’s safe.
Healthcare providers say visual aids help too. A simple chart showing “Antibiotic Time” and “Safe Antacid Time” taped to the fridge cuts timing errors by 37%.
Why This Matters Beyond Your Own Health
When antibiotics fail because of bad timing, people often go back to the doctor. They get another prescription. Then another. Each time, the bacteria are exposed to low doses of the drug - not enough to kill them, but enough to teach them how to survive. That’s how antibiotic resistance grows.The CDC estimates that 15% of new fluoroquinolone resistance cases in the U.S. can be traced back to subtherapeutic levels caused by antacid interactions. That’s not just your problem. It’s a public health issue.
And the cost? In the U.S. alone, unnecessary treatment failures from this interaction cost the healthcare system $1.2 billion a year. That’s billions in extra doctor visits, lab tests, and stronger antibiotics - all preventable.
Bottom Line: Timing Is Everything
You wouldn’t mix bleach and ammonia. You wouldn’t take aspirin if you’re allergic. And you shouldn’t take antacids and antibiotics together without spacing them out. This isn’t complicated. It’s basic. But it’s overlooked.If you’re on antibiotics and you have heartburn:
- Check the name of your antibiotic.
- Know if it’s a fluoroquinolone or tetracycline - those are the high-risk ones.
- Wait at least 2 hours, or 4 hours if it’s ciprofloxacin or levofloxacin.
- Ask your pharmacist - they’re trained to catch this.
- Consider switching to a different acid reducer if you need daily help.
One simple change - waiting a few hours - can make your antibiotic work like it’s supposed to. No extra pills. No stronger drugs. Just better timing.
Can I take Tums with amoxicillin?
Yes, but not right at the same time. Amoxicillin is less affected by antacids than other antibiotics. Taking Tums with it might reduce absorption by about 15-20%, but this rarely leads to treatment failure. Still, to be safe, wait at least 1-2 hours between doses. If you’re unsure, take the antibiotic first, then the antacid later.
What happens if I accidentally take my antibiotic with an antacid?
If you accidentally take them together once, don’t panic. One mistake won’t ruin your whole course. But don’t make it a habit. If you’re on a short course (like 5-7 days), you might still be okay. But if you’re on a longer course or have a serious infection (like a kidney or bone infection), contact your doctor. They may want to check your progress or switch you to a different antibiotic.
Does it matter if I take the antacid before or after the antibiotic?
Yes, it does. For high-risk antibiotics like ciprofloxacin, it’s best to take the antibiotic at least 2 hours before the antacid. This gives the antibiotic time to be absorbed before the antacid raises your stomach pH and starts binding minerals. If you take the antacid first, you need to wait 4 hours before taking the antibiotic. The earlier you take the antibiotic, the better.
Are all antacids the same?
No. Antacids with aluminum, magnesium, or calcium are the problem. Brands like Tums (calcium carbonate), Rolaids (calcium carbonate and magnesium hydroxide), and Maalox (aluminum and magnesium hydroxide) all cause interactions. Antacids with sodium bicarbonate (like Alka-Seltzer) are less likely to interfere, but they’re not ideal for daily use. Always check the active ingredients on the label.
Can I use antacids if I’m on metronidazole?
Yes. Metronidazole doesn’t interact with antacids. You can take them together without any timing concerns. This makes metronidazole a good option if you have frequent heartburn and need an antibiotic for infections like bacterial vaginosis or C. diff.
Should I stop taking antacids while on antibiotics?
Only if you can manage without them. If you have chronic acid reflux or ulcers, stopping antacids could make you feel worse and even interfere with healing. Instead of stopping, switch to a different type of acid reducer - like famotidine or omeprazole - that doesn’t interfere with antibiotics. Talk to your doctor or pharmacist before making any changes.


Mindee Coulter
January 28, 2026 AT 23:26Just took cipro yesterday and had a Tums after lunch. Felt like a genius until I read this. Thanks for the wake-up call. I’ll space it out now. 🙌
Mark Alan
January 30, 2026 AT 04:04AMERICA NEEDS TO STOP BEING LAZY WITH MEDS 😤 I take my antibiotics like a soldier - 4 hours apart, no excuses. If you can’t follow basic science, don’t blame the drug. Blame your phone alarm. 🇺🇸💊
Anna Lou Chen
February 1, 2026 AT 00:24Chelation isn’t just a biochemical event - it’s a metaphysical negotiation between the body’s demand for efficacy and the mind’s craving for comfort. The antacid, in its innocence, becomes a Trojan horse of homeostasis, disrupting the pharmacodynamic symphony. We mistake relief for resolution - and in doing so, we domesticate resistance.
Perhaps the real question isn’t ‘when to take it?’ but ‘why do we rely on band-aid chemistry at all?’
Bryan Fracchia
February 1, 2026 AT 18:17Wow, this is one of those posts that makes you feel like you’ve been doing everything right - and then realize you’ve been doing half of it right.
I’ve been taking doxycycline for acne and Tums for heartburn. Never thought about spacing them. I’ll start taking my antibiotic right after waking up, and my antacid after lunch. Small change, huge difference. Thanks for making this so clear.
Lance Long
February 3, 2026 AT 12:03You’re not alone. I’ve seen so many patients come in with the same story - ‘I did everything right, but it didn’t work.’ And then we ask about the Tums.
It’s not their fault. No one tells you this. Pharmacists don’t always bring it up. Doctors assume you know. But here’s the thing: you don’t need to be a scientist to save your own treatment. Just wait two hours. That’s it.
You got this. One pill at a time.
fiona vaz
February 4, 2026 AT 21:57Metronidazole + antacids = no problem. I’ve been doing it for years. If you’re on long-term antibiotics and need acid control, ask your doc about metronidazole as an alternative. It’s not always the first choice, but it’s a lifesaver for people like me with chronic reflux.
Also - MyMedSchedule app is legit. Set it up last month. It saved me from a second UTI.
Sue Latham
February 5, 2026 AT 23:57Ugh. Of course it’s the antacids. I mean, come on. If you’re popping Tums like candy and then wonder why your UTI won’t quit… you’re basically feeding the bacteria a free pass. 🤦♀️
And no, ‘I forgot’ isn’t an excuse. Your phone has a calendar. Use it. Or stop pretending you care about your health.
Robert Cardoso
February 6, 2026 AT 21:56Let’s be real - 15% of fluoroquinolone resistance traced to antacid interactions? That number is inflated. Most of those cases involve non-compliance, poor diagnostics, or overprescribing. The real issue is systemic antibiotic misuse, not a 2-hour window. This post is fear-mongering dressed as education.
Also, ‘Cipro XR-24’? That’s not a real formulation. You’re making that up.
Kathy Scaman
February 7, 2026 AT 13:20My grandma takes Tums with everything. She just found out she’s been doing it wrong with her antibiotics. Now she’s got a sticky note on her pillbox that says ‘ANTIBIOTIC FIRST, TUMS LATER.’
She’s 78. She got it. You can too.
Linda O'neil
February 9, 2026 AT 08:16If you’re on antibiotics and you’re still getting heartburn - don’t just reach for the antacid. Try eating smaller meals. Avoid spicy food. Sleep propped up. Your body can heal without chemicals. But if you need the antacid? Wait 2-4 hours. It’s not hard. It’s just new.
You’re not failing. You’re learning.
John Rose
February 10, 2026 AT 04:17One sentence: If you take ciprofloxacin and Tums together, you’re basically flushing $80 down the toilet and risking a resistant infection. Just wait 4 hours. It’s that simple.